Resident Readiness General Surgery (34 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

TIPS TO REMEMBER
Delirium can be the first sign of a life-threatening medical condition.
The first principle in managing delirium is to diagnose and reverse the underlying cause.
A review of the entire medication list for offending agents should be completed. Medications including anticholinergic agents, benzodiazepines, and opiates are common contributors to delirium and should be reduced if possible.
Dopamine antagonists (ie, IV haloperidol) are useful first-line pharmacologic agents for the treatment and management of delirium.
COMPREHENSION QUESTIONS
1.
Which of the following is most helpful in securing a diagnosis of delirium as the cause of mental status changes?
A. Paranoid delusions
B. Altered level of consciousness with impaired cognition
C. Agitation
D. Perceptual disturbances
E. Concurrent use of opiates and benzodiazepines
2.
Of the following which would
not
be a first-line recommendation in the management of delirium?
A. Provide visual/hearing aids.
B. Reverse underlying medical etiology.
C. Intravenous haloperidol PRN agitation.
D. Diphenhydramine in the evening to optimize the sleep/wake cycle.
3.
What risk factors does the patient in the vignette possess for the development of delirium?
A. Anemia
B. The second postoperative day
C. Presence of leukocytosis
D. Burn injuries
E. Metabolic derangements
F. All of the above
Answers
1.
B
. The core feature of delirium is an altered level of consciousness with impaired cognition. All of the other symptoms listed are associated with delirium but not necessary for diagnosis.
2.
D
. Although optimizing the sleep/wake cycle is important, diphenhydramine has strong anticholinergic properties and as such would not be a first choice in a patient with AMS.
3.
F
. Anemia, metabolic derangements, and the presence of leukocytosis all contribute to an increased probability of transitioning to delirium. In addition, as outlined above, burn-related injuries and postoperative states may result in a pro-inflammatory cytokinemediated process that leads to CNS dysfunction, resulting in encephalopathy.
 You (the Intern) Are Asked to Read a Chest X-ray
You (the Intern) Are Asked to Read a Chest X-ray
Alexander T. Hawkins, MD, MPH and Amy Robin Deipolyi, MD, PhD
You are in Tuesday morning trauma rounds after a night shift. The room is warm, and the senior’s voice is monotonous. You begin to drift off to sleep when you hear your name called to go to the front of the room to read a chest x-ray. You know nothing about the patient. Where do you start?
1.
What is the first thing you should do with the chest x-ray?
2.
What is an easy acronym you can use to recall all of the important parts of the chest x-ray?
3.
What else do you need to look for on an ICU film?
HOW TO READ A CHEST X-RAY
Answers
The key to reading a chest x-ray is to develop a system that you will be able to replicate time after time. This will ensure that you evaluate every important aspect of the chest x-ray consistently. If you are not looking for it, you are not going to see it! What follows is an example of such a system. It is by no means the only way to look at a chest x-ray, and you should develop your own system that works for you.
1.
Make sure that it is hung (or displayed) correctly and that it is a chest x-ray of the correct patient. Sometimes images get mixed up or the side is incorrectly marked. Look for the heart on the left side of the chest (unless, of course, the patient has dextrocardia). Make sure that it has appropriate exposure and that you can see everything that you need to see (ie, apices of lungs, costophrenic angles). On a properly exposed film, the lungs are not too black and you can see the vertebral bodies through the heart. Ideally, patients are imaged straight on, rather than being rotated, which can distort the appearance of the mediastinum. Additionally, adequate inspiration is essential to good technique. In adults, approximately 9 posterior ribs should be identified. Low lung volumes mimic pulmonary edema.
2.
Just like a trauma evaluation, ABCDE can be used to note each important part of the radiograph. This method takes advantage of the fact that all you want to
do when you look at a chest x-ray is look at the lungs—which is why it saves the lungs for last.
A—Abdomen. Look for free air under the abdomen on an upright film.
B—Bones. Examine all of the ribs, clavicles, and vertebrae for fractures or dislocations.
C—Cardiac. Trace the cardiac silhouette starting from the right base, along the right atrium, and examine the mediastinum for any tumors or deviation. Evaluate the aortic arch on the left and trace the silhouette down to the left ventricle. On a PA CXR you can measure the width of the heart and compare it with the width of the chest. A ratio greater than 1:2 is evidence of cardiomyopathy. This rule does not apply to a portable AP CXR, which magnifies the mediastinum and heart.
D—Diaphragm. This one is really about the pleura, but ABCPE does not really make sense. Start at the diaphragm and trace the pleura all the way around the thoracic cavity. Blunting of the costophrenic angles can indicate a pleural effusion. Increased lucency and/or lines where they don’t belong can indicate a pneumothorax. Look especially hard in the apices of the lungs for this, although air can accumulate more inferiorly in patients who are supine. Look for a deep sulcus sign in supine patients, for example, in an ICU setting, which appears as a long pointed costophrenic angle.
E—Everything else. Now it is time to look at the lungs. Start with the trachea. Is it midline? Are any of the lobes opacified? Are there any tumors? Make sure you scan throughout the right and left lungs. Classic blind spots are the lung apices and lung behind the heart. Also note the pattern of an abnormal opacity. Is the process diffuse or localized? More central or peripheral? Hazy or linear? Does the opacity obscure a normal silhouette? For example, opacities that block the left or right heart borders represent an abnormality in the lingula or right middle lobe, respectively, whereas opacities obscuring either diaphragm are in the lower lobes. See
Figure 25-1
.
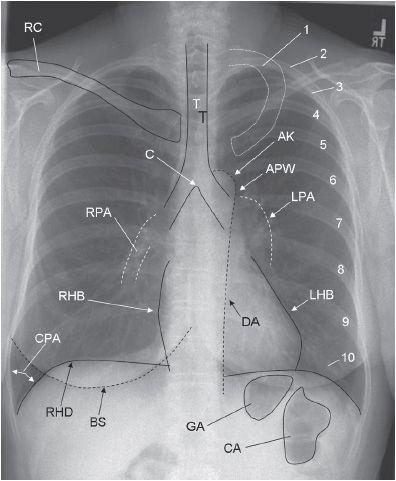
Figure 25-1.
Structures seen on a posteroanterior (PA) chest x-ray. 1, first rib; 2–10, posterior aspect of ribs 2 to 10; AK, aortic knob; APW, aortopulmonary window; BS, breast shadow (labeled only on right); C, carina; CA, colonic air; CPA, costophrenic angle; DA, descending aorta; GA, gastric air; LHB, left heart border (
Note
: Most of the left heart border represents the left ventricle; the superior aspect of the left heart border represents the left atrial appendage); LPA, left pulmonary artery; RC, right clavicle (left clavicle not labeled); RHB, right heart border (
Note
: The right heart border represents the right atrium); RHD, right hemidiaphragm (left hemidiaphragm not labeled); RPA, right pulmonary artery; T, tracheal air column.
