Resident Readiness General Surgery (13 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

1.
Which of the following findings is
not
needed to make the diagnosis of acute cholecystitis?
A. RUQ pain
B. RUQ tenderness
C. Gallstones on ultrasound
D. Systemic signs of infection (fever, leukocytosis, etc)
2.
A patient has an elevated white count, elevated bilirubin, and stones seen on a RUQ ultrasound. What other lab do you need to order?
A. Alkaline phosphatase
B. Lipase
C. AST
D. CRP
3.
A 40-year-old obese female presents to the ED with RUQ pain and tenderness but a normal white count and no fevers. A RUQ ultrasound is somewhat limited by the patient’s body habitus, but from what the ultrasonographer could see the patient didn’t have any stones or any signs of inflammation. What is the next step?
A. Book the OR and obtain the patient’s consent for a laparoscopic cholecystectomy.
B. Send her home with precautions to return if she develops a fever.
C. Admit her and begin IV antibiotics.
D. Obtain a HIDA scan.
Answers
1.
C
. If a patient has all 3 features of the “diagnostic triangle,” ultrasound is not needed.
2.
B
. The patient almost certainly has a stone that is obstructing biliary outflow. The only question that remains is whether or not it is also obstructing pancreatic outflow, and therefore if the patient’s pain might be due to (gallstone) pancreatitis.
3.
D
. This is the perfect indication for a HIDA scan—a decent story but not all 3 features of the “diagnostic triangle.”
 A 23-year-old Student With Periumbilical Pain That Has Migrated to Her RLQ
A 23-year-old Student With Periumbilical Pain That Has Migrated to Her RLQ
Brian C. George, MD and Alden H. Harken, MD
Megan O’Flaherty is a 23-year-old graduate student with a 36-hour history of periumbilical pain that has migrated to her RLQ. She states that she has felt febrile and is nauseated but denies vomiting or diarrhea. She is sexually active with a single partner and her last menstrual period was 2 weeks ago.
She denies prior hospitalizations and her only medications are birth control pills.
On physical examination, her vital signs are:
Temperature: 38.5°C
Blood pressure: 130/80
Heart rate: 80 (regular)
Respirations: 18
Finger oximetry: 98.5% (room air)
Abdominal examination reveals RLQ tenderness without rebound and hypo-active bowel sounds. Pelvic examination reveals right adnexal tenderness without cervical discharge or motion tenderness. Rectal examination confirms RLQ tenderness and brown, soft, guaiac-negative stool.
Your working diagnosis is: acute abdomen, rule out appendicitis.
1.
What findings support the diagnosis of appendicitis?
2.
What confirmatory laboratory tests are indicated?
3.
Are any imaging studies indicated?
4.
What is the next therapeutic step?
5.
What are the next steps if, at surgery, you find a normal appendix?
6.
What if the RLQ pain developed over days and weeks instead of hours?
RLQ PAIN
Answers
1.
Ms. O’Flaherty has clearly read the textbook chapter on appendicitis. Her pain developed over 36 hours and began with visceral (appendiceal) irritation that she perceived as midline discomfort. As her appendiceal inflammation became
transmural, she stimulated somatic peritoneal nerves sufficient to cause RLQ pain but not sufficient to cause rebound. “Rebound” can be elicited by pressing very gently on the RLQ and then releasing the pressure. When the inflamed visceral and parietal peritoneum rub against each other, this causes discomfort. If the patient winces during this procedure, he or she has an inflamed peritoneal surface.
As with all patients, the history and physical examination can help you narrow the differential. For example, if this patient had recently eaten at an unfamiliar ethnic restaurant and now had raging diarrhea, you would think more of gastroenteritis. If she had a cervical discharge and exquisite tenderness with cervical motion (chandelier sign), you would think of pelvic inflammatory disease (PID).
2.
(A) Obtain a CBC with differential. The Surviving Sepsis Campaign defines a “septic state” as WBC less than 4000 or greater than 12,000. We obtain a hemoglobin, hematocrit, and platelets probably because it is part of the “CBC package” (and, because “we have always done it that way”).
(B) A normal menstrual period 2 weeks ago does not preclude pregnancy. A serum HCG is an exquisitely sensitive test and should be obtained.
3.
Calculating an Alvarado score (which does not, unfortunately, include C-reactive protein) can help you decide whether you need additional confirmatory data or if you can take the patient directly to the OR (
Table 10-1
).
Table 10-1.
Calculation of an Alvarado Score
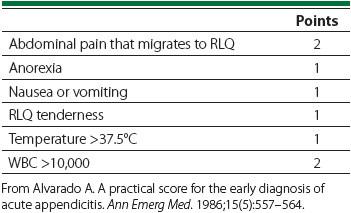
A French group (Pouget-Baudry et al) took patients with an Alvarado score of ≥6 directly to the OR and found 3 of 174 “negative” appendices. This group safely “watched” patients with <4 points. A Dutch group (Ünlü et al) evaluated routine diagnostic imaging in patients with appendicitis and reported diagnostic accuracy of ultrasound 71% and CT scan 95%.
4.
Take the patient to the operating room with the preoperative diagnosis of “acute abdomen,” not “appendicitis.” Give antibiotics to cover colonic gram-negatives
and anaerobes (such as ciprofloxacin and Flagyl, or cefotetan), and prepare for a laparoscopic RLQ exploration.
5.
Darn—but, in young females (this is the highest-risk group) it is permissible to bat 80%. After viewing a perfectly healthy appendix, you should fall back upon a routine series of exploratory steps:
A. If the right adnexa is socked in with inflammation, the diagnosis is PID and should be treated with IV antibiotics.
B. In young women, a large ovarian cyst is most likely to contain old blood (chocolate cysts) and is unlikely to harbor cancer. If you want to be conscientious, you may ultrasound the cyst looking for solid tissue (indicative of cancer). If you suspect ovarian cancer (usually in the middle of the night), this is not an emergency, and it is permissible to close and obtain GYN consultation. When a cyst reaches 6 to 8 cm, there is a risk of torsion, and this ovary should be “pexed” to the pelvic side wall.
C. If halfway down the Fallopian tube you see a walnut-sized bulge, you must suspect an ectopic pregnancy. The appropriate response is to make a linear incision in the tube and scoop out the ectopic fetus (do not perform a salpingectomy). Then close loosely with absorbable sutures.
D. When the GYN organs also appear healthy, redirect your attention to the terminal ileum (TI). In 2% of patients, 2 ft proximal to the TI, a Meckel diverticulum will become inflamed (rule of 2s). A narrow-neck Meckel diverticulum with thick tissue in the fundus (ectopic gastric mucosa) should be resected (either staple the neck or sleeve resection of the ileum). A wide-based diverticulum with no ectopic tissue may be safely left alone.
E. Inspect the terminal ileum for boggy, edematous, “creeping” mesenteric fat involvement indicative of Crohn disease. In the absence of intestinal obstruction (which Megan doesn’t have), don’t poke a skunk—leave this alone. If this inflammatory process does not appear to involve the base of the appendix, however, remove the appendix.
F. Having interrogated the “usual suspects,” you should remove the appendix—but there is 1 remaining “curve ball.” If you find a tan mass at the base of the appendix, you must suspect a carcinoid tumor. Carcinoids may exist anywhere in the GI tract from mouth to anus, but 60% present in the appendix. Most are benign. When the tumor reaches 2 cm in diameter, especially if it appears to invade the mesoappendix, it is considered malignant, obligating a right hemicolectomy.
6.
Some stoic patients will tough it out through a bout of appendicitis and even appendiceal rupture. They present with chronic RLQ discomfort, and your first step is a CT scan looking for loculated “drainable” pus that is accessible by interventional radiology. A RLQ phlegmon with no abscess is treated with
IV antibiotics. The issue of late “interval” appendectomy is controversial and hospital specific.
TIPS TO REMEMBER
The location of pain and tenderness helps you narrow the differential dramatically—focal tenderness suggests local inflammation of the peritoneum.
The Alvarado score can be used to gauge the probability that a patient has acute appendicitis. If less than 4, acute appendicitis is unlikely and observation is a reasonable approach. If greater than 6, then acute appendicitis is very likely. For borderline cases or unusual presentations, imaging can be helpful.
The differential for RLQ pain includes acute appendicitis, inflammatory bowel disease, Meckel diverticulum, ectopic pregnancy, ovarian cyst and/or torsion, PID, or cancer (eg, carcinoid).
