Resident Readiness General Surgery (12 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

2.
Which of those diseases commonly cause RUQ tenderness?
3.
What distinguishes a positive Murphy sign from simple RUQ tenderness?
4.
In the case above, can you pick out the 3 clinical features that most strongly support the diagnosis of acute cholecystitis?
5.
If this patient has an elevated serum bilirubin, what do you need to look for?
6.
Assume that his lab values were consistent with acute cholecystitis. If an ultrasound was equivocal, what would you do next?
RUQ PAIN
Answers
1.
All RUQ pain is not cholecystitis—although it will sometimes seem like it. While other causes
are
less common, the differential for RUQ pain is still moderately broad. To generate the differential, one approach is to think anatomically:
•
Stomach/duodenum: peptic ulcer disease
•
Biliary collecting system: biliary obstruction (eg, from a stone or a pancreatic mass)
•
Pancreas: pancreatitis
•
Liver: hepatitis
•
Gallbladder: plain ol’ biliary colic, acute cholecystitis
Biliary colic can sometimes be confusing because, like acute cholecystitis, it is also caused by gallstones. Biliary colic, however, is not an inflammatory process—hence the reason that it does not have an “-itis” in the name. Instead, it is caused by a gallstone
transiently
obstructing outflow from the gallbladder. This is perceived as visceral pain that refers to the epigastrium. If, on the other hand, the stone gets stuck and the obstruction therefore persists, the resulting stasis and increased pressure eventually lead to cholecystitis and associated somatic pain in the RUQ.
2.
Focal abdominal tenderness is usually caused by an inflammatory process that will involve the peritoneum. When that peritoneum is irritated by your palpation, the patient feels somatic pain, that is, pain localized to where you are palpating. We call that
focal
peritonitis. So, to rephrase this question: which of the above diseases commonly cause
focal
RUQ peritonitis? Clearly, acute cholecystitis is one culprit. Hepatitis can also cause some adjacent peritoneal inflammation. As described above, biliary colic is an obstructive and not an inflammatory condition, and hence causes visceral pain but no focal peritonitis.
3.
A positive Murphy sign is
cessation of inspiration
when the examiner’s hand comes in contact with the gallbladder. It is a physical exam maneuver that elicits somatic pain in the RUQ. It is performed by asking the patient to inspire while the examiner’s hand is placed inferior and deep to the liver edge, in a position where one would expect to find the gallbladder. With inspiration the abdominal contents are pushed down by the diaphragm that causes the gallbladder to move toward the examiner’s hand. If there is inflammation of the peritoneum overlying the gallbladder, the peritoneal somatic afferents will be stimulated when the examiner’s hand “touches” the gallbladder. This stimulation is perceived as sharp, localized somatic pain that causes the patient to abruptly halt inspiration.
4.
The key feature of cholecystitis is the inflammatory process. It is this inflammation that causes the 3 findings that together are highly suggestive of acute cholecystitis (see
Figure 9-1
):
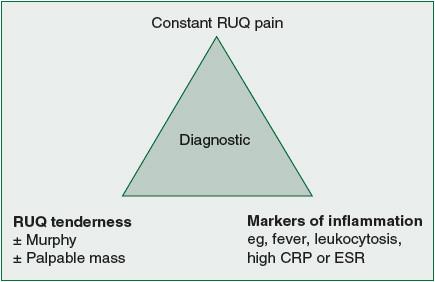
Figure 9-1.
The diagnosis of acute cholecystitis can be made if a patient has all three elements of the so-called diagnostic triangle. (Figure adapted from Indar AA, Beckingham IJ. Acute cholecystitis.
BMJ
. 2002;325(7365):639–643.)
•
Pain in the RUQ (
not
in the midline—remember that focal peritoneal inflammation causes localized
somatic
pain)
•
Tenderness in the RUQ (again, due to focal peritonitis)
•
Fevers and/or leukocytosis and/or elevated CRP (
more
evidence of inflammation!)
If you look back at the other diseases on the differential, only hepatitis would regularly cause RUQ somatic pain, RUQ tenderness, and systemic signs of inflammation. Fortunately, hepatitis is easily distinguished from cholecystitis by history and by routine laboratory studies—it isn’t usually associated with a significant leukocytosis, and the transaminases are markedly elevated. About one third of the time you cannot make a diagnosis on clinical information alone. In those circumstances imaging can help.
5.
Biliary obstruction—by ultrasound, ERCP, or MRCP. Clinically this patient has acute cholecystitis, and since 90% of acute cholecystitis is caused by gallstones, it is a fair assumption that he is at risk for dropping a stone into the common bile duct. If it gets hung up somewhere, it causes hyperbilirubinemia and can lead to an infection of the biliary tree (aka cholangitis). If it goes far enough down, it can also obstruct the pancreatic outflow and lead to pancreatitis. In other words, gallstones can cause 3 distinct disease entities, 2 of which are associated with hyperbilirubinemia.
6.
First, what does it mean to be “equivocal?” Or stated differently, what features are consistent with acute cholecystitis? We can divide ultrasound findings into 2 categories: causes of cholecystitis and effects of cholecystitis. The causes of cholecystitis that we look for on ultrasound would most commonly include gallstones, but might also include a mass either within or adjacent to the neck of the gallbladder (ie, cancer). Effects of cholecystitis that we might look for on ultrasound are the natural sequelae of inflammation, namely, a thickened gallbladder wall and pericholecystic fluid (both due to edema), as well as a so-called sonographic Murphy sign. See
Figure 9-2
.
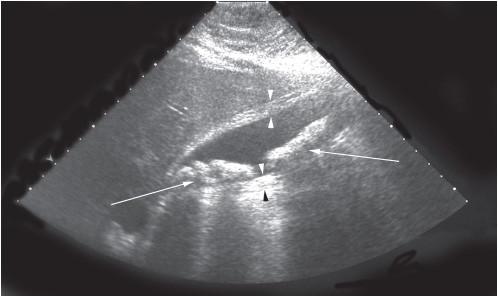
Figure 9-2.
In this ultrasound image we can clearly see hyperechoic masses as well as the shadowing indicated by the large arrow. (Reproduced with permission from Brunicardi FC, Andersen DK, Billiar TR, et al.
Schwartz’s Principles of Surgery.
9th ed. New York: McGraw-Hill; 2010 [Figure 32-14].)
While ultrasound is good, it is far from perfect. Sometimes you might suspect cholecystitis based on clinical features, but the story isn’t a slam dunk and the ultrasound doesn’t reveal any stones. What do you do? One option is to get a HIDA scan.
A HIDA scan is a nuclear scan in which bile is tagged with a mildly radioactive tracer. Because bile is normally sequestered in the gallbladder until a meal, the gallbladder should be filled with the radioactive bile and therefore clearly seen on the scan. If, on the other hand, the gallbladder is not seen, this indicates that it is “nonfilling,” that is, it has an inflow and therefore almost certainly an outflow obstruction. As we know from above, outflow obstruction is one of the key steps in the pathophysiology of acute cholecystitis, and therefore an absent gallbladder on HIDA scan is strongly suggestive of the disease.
TIPS TO REMEMBER
Acute cholecystitis is a clinical diagnosis that can often be made on the basis of RUQ pain, RUQ tenderness, and systemic signs of inflammation.
A positive Murphy sign is cessation of inspiration with deep palpation of the RUQ.
Besides biliary colic and acute cholecystitis, gallstones in the biliary tree can also cause cholangitis or gallstone pancreatitis.
Don’t forget the HIDA scan if the diagnosis remains uncertain after labs and an ultrasound.
COMPREHENSION QUESTIONS
