Ross & Wilson Anatomy and Physiology in Health and Illness (97 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Posterior pituitary
The structure of the posterior pituitary gland and its relationship with the hypothalamus is explained on
page 209
.
Oxytocin
and
antidiuretic hormone
(ADH or vasopressin) are the hormones synthesised in nerve cell bodies in the hypothalamus and then stored in the axon terminals within the posterior pituitary gland (
Fig. 9.3B
). These hormones act directly on non-endocrine tissue and their release from synaptic vesicles by exocytosis is stimulated by nerve impulses from the hypothalamus.
Oxytocin
Oxytocin stimulates two target tissues during and after childbirth (parturition): uterine smooth muscle and the muscle cells of the lactating breast.
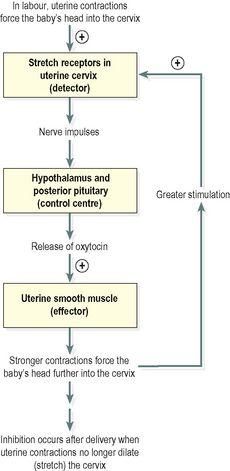
During childbirth increasing amounts of oxytocin are released by the posterior pituitary into the bloodstream in response to increasing distension of sensory stretch receptors in the uterine cervix by the baby’s head. Sensory impulses are generated and travel to the control centre in the hypothalamus, stimulating the posterior pituitary to release more oxytocin. In turn this stimulates more forceful uterine contractions and greater stretching of the uterine cervix as the baby’s head is forced further downwards. This is an example of a
positive feedback mechanism
which stops soon after the baby is delivered and distension of the uterine cervix is greatly reduced (
Fig. 9.5
).
Figure 9.5
Regulation of secretion of oxytocin through a positive feedback mechanism.
The process of milk ejection also involves a positive feedback mechanism. Suckling generates sensory impulses that are transmitted from the breast to the hypothalamus. The impulses trigger the release of oxytocin from the posterior pituitary and oxytocin stimulates contraction of the myoepithelial cells around the glandular cells and ducts of the lactating breast to contract, ejecting milk. Suckling also inhibits the release of
prolactin inhibiting hormone
(PIH), prolonging prolactin secretion and lactation. The role of this hormone in males and non-lactating females remains unclear.
Antidiuretic hormone (ADH, vasopressin)
The main effect of antidiuretic hormone is to reduce urine output (diuresis is the production of a large volume of urine). ADH acts on the distal convoluted and collecting ducts of the nephrons of the kidneys (
Ch. 13
), increasing their permeability to water. As a result, the reabsorption of water from the glomerular filtrate is increased. The amount of ADH secreted is determined by the osmotic pressure of the blood circulating to the
osmoreceptors
in the hypothalamus.
As the osmotic pressure rises, for example as a result of dehydration or following haemorrhage, the secretion of ADH increases. More water is therefore reabsorbed and the urine output is reduced. This means that the body retains more water and the rise in osmotic pressure is reversed. Conversely, when the osmotic pressure of the blood is low, for example after a large fluid intake, secretion of ADH is reduced, less water is reabsorbed and more urine is produced (
Fig. 9.11
).
At high concentrations, for example after severe blood loss, ADH causes smooth muscle contraction, especially vasoconstriction in small arteries. This has a
pressor effect
, raising systemic blood pressure; the alternative name of this hormone, vasopressin, reflects this effect.
Thyroid gland (
Fig. 9.6
)
Learning outcomes
After studying this section you should be able to:
describe the position of the thyroid gland and its related structures
describe the microscopic structure of the thyroid gland
outline the actions of the thyroid hormones
explain how blood levels of the thyroid hormones T
3
and T
4
are regulated.
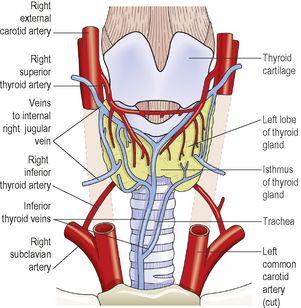
Figure 9.6
The position of the thyroid gland and its associated structures
. Anterior view.
The thyroid gland is situated in the neck in front of the larynx and trachea at the level of the 5th, 6th and 7th cervical and 1st thoracic vertebrae. It is a highly vascular gland that weighs about 25 g and is surrounded by a fibrous capsule. It resembles a butterfly in shape, consisting of two
lobes
, one on either side of the thyroid cartilage and upper cartilaginous rings of the trachea. The lobes are joined by a narrow
isthmus
, lying in front of the trachea.
The lobes are roughly cone shaped, about 5 cm long and 3 cm wide.
The
arterial blood supply
to the gland is through the superior and inferior thyroid arteries. The superior thyroid artery is a branch of the external carotid artery and the inferior thyroid artery is a branch of the subclavian artery.
The
venous return
is by the thyroid veins, which drain into the internal jugular veins.
Two parathyroid glands lie against the posterior surface of each lobe and are sometimes embedded in thyroid tissue. The recurrent laryngeal nerve passes upwards close to the lobes of the gland and on the right side it lies near the inferior thyroid artery (see
Fig. 9.9
).
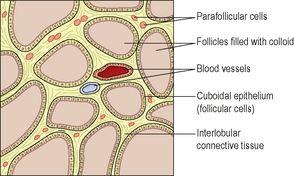
The gland is composed of cuboidal epithelium that forms spherical follicles. These secrete and store
colloid
, a thick sticky protein material (
Fig. 9.7
). Between the follicles there are other cells found singly or in small groups:
parafollicular cells
, also called C-cells, which secrete the hormone
calcitonin
.