Ross & Wilson Anatomy and Physiology in Health and Illness (43 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Factors determining blood pressure
Blood pressure is determined by
cardiac output
and
peripheral resistance
. Change in either of these parameters tends to alter systemic blood pressure, although the body’s compensatory mechanisms usually adjust for any significant change.
Cardiac output
Cardiac output is determined by the stroke volume and the heart rate (
p. 85
). Factors that affect the heart rate and stroke volume are described above, and they may increase or decrease cardiac output and, in turn, blood pressure. An increase in cardiac output raises both systolic and diastolic pressures. An increase in stroke volume increases systolic pressure more than it does diastolic pressure.
Peripheral or arteriolar resistance
Arterioles are the smallest arteries and they have a tunica media composed almost entirely of smooth muscle, which responds to nerve and chemical stimulation. Constriction and dilation of the arterioles are the main determinants of peripheral resistance (
p. 76
). Vasoconstriction causes blood pressure to rise and vasodilation causes it to fall.
When elastic tissue in the tunica media is replaced by inelastic fibrous tissue as part of the ageing process, blood pressure rises.
Autoregulation
Systemic blood pressure rises and falls constantly, according to levels of activity, body position, etc. However, the organs of the body are capable of adjusting blood flow and blood pressure in their own local vessels independently of systemic blood pressure. This property is called
autoregulation
, and protects the tissues against swings in systemic pressures. It is especially important in the kidneys, which can be damaged by increased pressure in their delicate glomerular capillary beds (
pp. 331–332
), and in the brain, which is very sensitive to even slight levels of cellular waste.
Control of blood pressure (BP)
Blood pressure is controlled in two ways:
•
short-term control, on a moment-to-moment basis, which mainly involves the baroreceptor reflex, discussed below, and also chemoreceptors and circulating hormones
•
long-term control, which involves regulation of blood volume by the kidneys and the renin–angiotensin– aldosterone system (
p. 338
).
Short-term blood pressure regulation
The cardiovascular centre (CVC) is a collection of interconnected neurones in the medulla and pons of the brain stem. The CVC receives, integrates and coordinates inputs from:
•
baroreceptors (pressure receptors)
•
chemoreceptors
•
higher centres in the brain.
The CVC sends autonomic nerves (both sympathetic and parasympathetic) to the heart and blood vessels. It controls BP by slowing down or speeding up the heart rate and by dilating or constricting blood vessels. Activity in these fibres is essential for control of blood pressure (
Fig. 5.24
). The two divisions of the autonomic nervous system, the sympathetic and the parasympathetic divisions, are described more fully in
Chapter 7
. Their actions relating to the heart and blood vessels are summarised in
Table 5.1
.
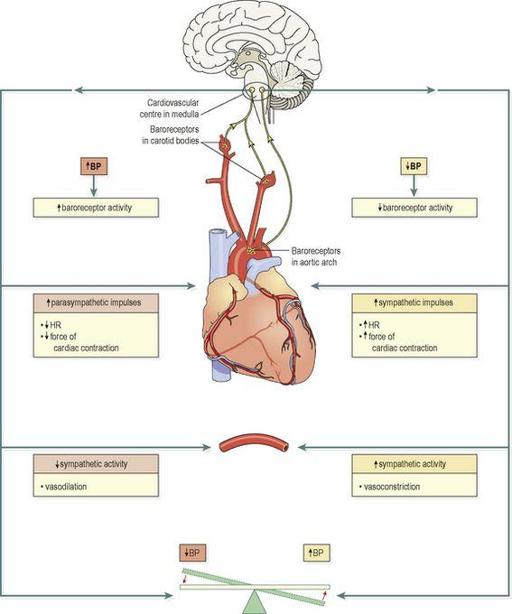
Figure 5.24
Summary of the main mechanisms in blood pressure control.
Table 5.1
The effects of the autonomic nervous system on the heart and blood vessels
| | Sympathetic stimulation | Parasympathetic stimulation |
|---|---|---|
| Heart | ↑rate | ↓rate |
| | ↑strength of contraction | ↓strength of contraction |
| Blood vessels | Most constrict, but arteries supplying skeletal muscle and brain dilate | Most blood vessels do not have a parasympathetic blood supply |
Baroreceptors
These are nerve endings sensitive to pressure changes (stretch) within the vessel, situated in the arch of the aorta and in the carotid sinuses (
Fig. 5.25
), and are the body’s principal moment-to-moment regulatory mechanism for controlling blood pressure. A rise in blood pressure in these arteries stimulates the baroreceptors, increasing their input to the CVC. The CVC responds by increasing parasympathetic nerve activity to the heart; this slows the heart down. At the same time, sympathetic stimulation to the blood vessels is inhibited, causing vasodilation. The net result is a fall in systemic blood pressure. Conversely, if pressure within the aortic arch and carotid sinuses falls, the rate of baroreceptor discharge also falls. The CVC responds by increasing sympathetic drive to the heart to speed it up. Sympathetic activity in blood vessels is also increased, leading to vasoconstriction. Both these measures counteract the falling blood pressure. Baroreceptor control of blood pressure is also called the
baroreceptor reflex
(
Fig. 5.25
).
Figure 5.25
The baroreceptor reflex.
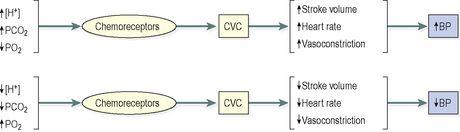
Chemoreceptors
These are nerve endings situated in the carotid and aortic bodies, and are primarily involved in control of respiration (
p. 252
). They are sensitive to changes in the levels of carbon dioxide, oxygen and the acidity of the blood (pH) (
Fig. 5.26
). Rising blood CO
2
, falling blood O
2
levels and/or falling pH all indicate failing tissue perfusion. When these changes are detected by the chemoreceptors, they send signals to the CVC, which then increases sympathetic drive to the heart and blood vessels, pushing blood pressure up to improve tissue blood supply. Because respiratory effort is also stimulated, blood oxygen levels rise as well.
Figure 5.26
The relationship between stimulation of chemoreceptors and arterial blood pressure.
Chemoreceptor input to the CVC influences its output only when severe disruption of respiratory function occurs or when arterial BP falls to less than 80 mmHg. Similar chemoreceptors are found on the brain surface in the medulla oblongata, and they measure carbon dioxide/oxygen levels and pH of the surrounding cerebrospinal fluid. Changes from normal activate responses similar to those described above for the aortic/carotid receptors.
Higher centres in the brain
Input to the CVC from the higher centres is influenced by emotional states such as fear, anxiety, pain and anger that may stimulate changes in blood pressure.
The hypothalamus in the brain controls body temperature and influences the CVC, which responds by adjusting the diameter of blood vessels in the skin – an important mechanism in determining heat loss and retention (
p. 357
).
Long-term blood pressure regulation
Long-term blood pressure control is mainly exerted by the
renin–angiotensin–aldosterone
system (RAAS, see
p. 338
) and the action of
antidiuretic hormone
(ADH, see
p. 335
). Both of these systems regulate blood volume, thus influencing blood pressure. In addition,
atrial natriuretic peptide
(ANP,
p. 336
), a hormone released by the heart itself, causes sodium and water loss from the kidney and reduces blood pressure, opposing the activities of both ADH and the RAAS.
Pressure in the pulmonary circulation
Pulmonary blood pressure is much lower than in the systemic circulation, because although the lungs receive the same amount of blood from the right ventricle as the rest of the body receives from the left ventricle, there are so many capillaries in the lungs that pressure is kept low. If pulmonary capillary pressure exceeds 25 mmHg, fluid is forced out of the bloodstream and into the airsacs (
pulmonary oedema
), with very serious consequences. Autoregulation in the pulmonary circulation makes sure that blood flow through the vast network of capillaries is directed through well-oxygenated airsacs (
p. 252
).
Pulse
Learning outcomes
After studying this section, you should be able to:
define the term pulse