Ross & Wilson Anatomy and Physiology in Health and Illness (151 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

This infection of the large intestine is caused by bacteria of the
Shigella
group. The severity of the condition depends on the organisms involved. In the UK it is usually a relatively mild condition caused by
Shigella sonnei
.
Shigella dysenteriae
causes the most severe type of infection and it occurs mainly in tropical countries. Children and elderly debilitated adults are particularly susceptible. The only host is humans and the organisms are spread by faecal contamination of food, drink, hands and fomites.
The intestinal mucosa becomes inflamed, ulcerated and oedematous with excess mucus secretion. In severe infections, the acute diarrhoea, containing blood and excess mucus, causes dehydration, electrolyte imbalance and anaemia. When healing occurs the mucous membrane is fully restored.
Amoebic dysentery (amoebiasis)
This disease is caused by
Entamoeba histolytica
. The only known hosts are humans and it is spread by faecal contamination of food, water, hands and fomites. Although many infected people do not develop symptoms they may become asymptomatic carriers. Within the colon, the amoebae grow, divide and invade the mucosal cells, causing inflammation. Without treatment the condition frequently becomes chronic with mild, intermittent diarrhoea and abdominal pain. This may progress with ulceration of the colon accompanied by persistent and debilitating diarrhoea that contains mucus and blood. Complications are unusual but include severe haemorrhage from ulcers and liver abscesses.
Viral gastroenteritis
Several viruses, including rotavirus and norovirus, are known to cause vomiting and/or diarrhoea. Rotavirus is a major cause of diarrhoea in young children. It is easily spread in healthcare facilities. Norovirus, also known as the ‘
winter vomiting virus
’, is responsible for outbreaks that commonly occur in winter causing short-lived and self-limiting enteritis with vomiting as the main symptom. It spreads easily in families and in child and healthcare facilities. Spread is by the faecal–oral route but airborne transmission by inhalation may also occur.
Inflammatory bowel disease (IBD)
This term includes Crohn’s disease and ulcerative colitis. A comparison of the main features is shown in
Table 12.4
. Their aetiology is unknown but is thought to involve environmental and immune factors in genetically susceptible individuals. Both conditions typically have a pattern of relapse and remission.
Table 12.4
Comparison of the main features of Crohn’s disease and ulcerative colitis
| | Crohn’s disease | Ulcerative colitis |
|---|---|---|
| Incidence | Usually between 20 and 40 years of age (mean 26 years); both sexes affected equally; smokers at higher risk | Usually between 20 and 40 years of age (mean 34 years); more women affected than men; smoking not a risk factor |
| Main sites of lesions | Anywhere in digestive tract from mouth to anus; common in terminal ileum | Rectum always involved, with variable spread along colon |
| Tissue involved | Entire thickness of the wall inflamed and thickened tissue; ulcers and fistulae common | Only mucosa involved |
| Nature of lesions | ‘Skip’ lesions, i.e. diseased areas interspersed with regions of normal tissue; ulcers and fistulae common | Continuous lesion; mucosa is red and inflamed |
| Prognosis | In severe cases, surgery may improve condition, but relapse rate very high, slightly increased risk of cancer | Surgical removal of entire colon cures the condition, significantly increased risk of cancer |
Crohn’s disease
This chronic inflammatory condition of the alimentary tract, also known as regional ileitis, usually occurs in young adults. The terminal ileum and the rectum are most commonly affected but the disease may affect any part of the tract. There is chronic patchy inflammation with oedema of the full thickness of the intestinal wall, causing partial obstruction of the lumen, sometimes described as
skip lesions
. There are periods of remission of varying duration. The main symptoms are diarrhoea, abdominal pain and weight loss. Complications include:
•
secondary infections, occurring when inflamed areas ulcerate
•
fibrous adhesions and subsequent intestinal obstruction caused by the healing process
•
fistulae between intestinal lesions and adjacent structures, e.g. loops of bowel, surface of the skin (
p. 361
)
•
perianal fistulae, fissures and skin tags
•
cancer of the small or large intestine.
Ulcerative colitis
This is a chronic inflammatory disease of the mucosa of the colon and rectum, which may ulcerate and become infected. It usually occurs in young adults and begins in the rectum and sigmoid colon. From there it may spread proximally to involve a variable proportion of the colon and, sometimes, the entire colon. The main symptom is bloody diarrhoea. There are periods of remission lasting weeks, months or years. Individuals may develop other systemic problems affecting, for example, the joints (ankylosing spondylitis,
p. 423
), skin and liver. In long-standing cases, cancer sometimes develops.
Toxic megacolon
is an acute complication where the colon loses its muscle tone and dilates. There is a high risk of electrolyte imbalance, perforation and hypovolaemic shock, which may be fatal if untreated.
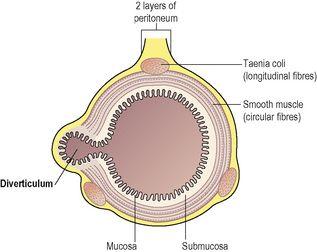
Diverticular disease
Diverticula are small pouches of mucosa that protrude (herniate) into the peritoneal cavity through the circular muscle fibres of the colon between the taeniae coli (
Fig. 12.50
). The walls consist of mucous membrane with a covering of visceral peritoneum. They occur at the weakest points of the intestinal wall, i.e. where the blood vessels enter, most commonly in the sigmoid colon.
Figure 12.50
Diverticular disease; cross-section of bowel showing one diverticulum.
The causes of
diverticulosis
(presence of diverticuli) are not known but it is associated with deficiency of dietary fibre. In Western countries, diverticulosis is fairly common after the age of 60 but diverticulitis affects only a small proportion.
Diverticulitis
arises when faeces impact in the diverticula and the walls become inflamed and oedematous as secondary infection develops. This reduces the blood supply causing ischaemic pain. Occasionally, rupture occurs resulting in peritonitis (
p. 317
).
Tumours of the small and large intestines
Benign and malignant tumours of the small intestine are rare, especially compared with their occurrence in the stomach, large intestine and rectum.
Benign tumours
Benign neoplasms may form a broad-based mass or polyp, i.e. develop a pedicle. Occasionally polyps twist upon themselves, causing ischaemia, necrosis and possibly gangrene. Malignant changes may occur in adenomas, which are mostly found in the large intestine. The incidence is high in developed countries.
Colorectal cancer
This is the most common malignancy of the alimentary tract in Western countries and as a cause of cancer-related death is second only to lung cancer in the UK. The tumours are adenocarcinomas with about half arising in the rectum, one-third in the sigmoid colon and the remainder elsewhere in the colon.
The tumour may be:
•
a soft polypoid mass, projecting into the lumen of the colon or rectum with a tendency to ulceration, infection and bleeding
•
a hard fibrous mass encircling the colon, causing narrowing of the lumen and, eventually, obstruction.
The most important predisposing factor for colorectal cancer is thought to be diet. In cultures eating a high-fibre, low-fat diet, the disease is virtually unknown, whereas in Western countries, where large quantities of red meat and saturated animal fat and insufficient fibre are eaten, the disease is much more common. Slow movement of bowel contents may result in conversion of unknown substances present into carcinogenic agents. Genetic factors are also implicated. Predisposing diseases include ulcerative colitis and some benign tumours (usually adenomas).
Local spread
of intestinal tumours occurs early but may not be evident until there is severe ulceration and haemorrhage or obstruction. Spread can be outwards through the wall into the peritoneal cavity and adjacent structures.
Lymph-spread
metastases occur in mesenteric lymph nodes, the peritoneum and other abdominal and pelvic organs. Pressure caused by enlarged lymph nodes may cause obstruction or damage other structures.
Blood-spread
metastases are most common in the liver, brain and bones.
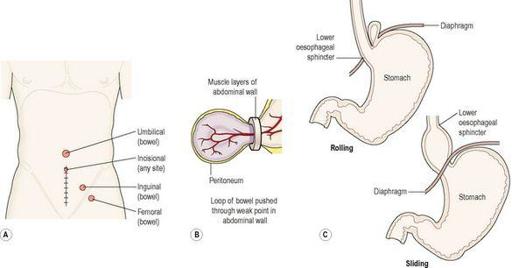
Hernias
A hernia is a protrusion of an organ or part of an organ through a weak point or aperture in the surrounding structures. In those affecting the digestive system, a piece of bowel protrudes through a weak point in either the musculature of the anterior abdominal wall or an existing opening (
Fig. 12.51A
). It occurs when there are intermittent increases in intra-abdominal pressure, most commonly in men who lift heavy loads at work. The underlying causes of the abdominal wall weakness are unknown. Outcomes include:
•
spontaneous reduction, i.e. the loop of bowel slips back to its correct place when the intra-abdominal pressure returns to normal
•
manual reduction, i.e. by applying gentle pressure over the abdominal swelling
•
strangulation
(
Fig. 12.51B
), when reduction is not possible and the venous drainage from the herniated loop of bowel is obstructed, causing congestion, ischaemia and gangrene. In addition there is intestinal obstruction (
p. 322
).
Figure 12.51
Hernias: A.
Common sites of herniation.
B.
Strangulated hernia formation.
C.
Hiatus hernia.
Sites of hernias (
Fig. 12.51A
)
Inguinal hernia
The weak point is the inguinal canal, which contains the spermatic cord in the male and the round ligament in the female. It occurs more commonly in males than in females.
Femoral hernia
The weak point is the femoral canal through which the femoral artery, vein and lymph vessels pass from the pelvis to the thigh.
Umbilical hernia
The weak point is the umbilicus where the umbilical blood vessels from the placenta entered the fetus before birth.
Incisional hernia
This is caused by repeated stretching of fibrous tissue formed after previous abdominal surgery.
Hiatus hernia
This is the protrusion of a part of the fundus of the stomach through the oesophageal opening in the diaphragm (
Fig. 12.51C
). Although often asymptomatic, irritation of the oesophagus only occurs when there is reflux of acid gastric juice, especially when the individual lies flat or bends down. The long-term effects may be oesophagitis, fibrosis and narrowing of the oesophagus, causing dysphagia. Strangulation does not occur.
Rolling hiatus hernia