Ross & Wilson Anatomy and Physiology in Health and Illness (147 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Learning outcomes
After studying this section, you should be able to:
outline the pathophysiology of mumps
explain the nature of salivary calculi
describe the most common tumours of the salivary glands.
Mumps
This is an acute inflammatory condition of the salivary glands, especially the parotids. It is caused by the mumps virus, one of the parainfluenza group. The virus is inhaled in infected droplets and, during the 18- to 21-day incubation period, viruses multiply elsewhere in the body before spreading to the salivary glands. The virus is present in saliva for about 7 days before and after symptoms appear so the infection may spread to others during this 2-week period. Viruses also occasionally spread to:
•
the pancreas, causing pancreatitis
•
the testes, causing orchitis (testicular inflammation) after puberty and sometimes atrophy of the glands and sterility
•
the brain, causing meningitis (see
Ch. 7
) or meningoencephalitis.
In developed countries, children are usually vaccinated against mumps in their preschool years.
Calculus formation
Calculi (stones) are formed in the salivary glands by the crystallisation of mineral salts in saliva. They may partially or completely block the ducts, leading to inflammation and swelling of the gland, a predisposition to infection and, in time, atrophy. The causes are not known.
Tumours of the salivary glands
Mixed tumours (pleomorphic salivary adenoma)
This benign tumour consists of epithelial and connective tissue cells and occurs mainly in the parotid gland. It is the most common tumour of the salivary glands. A second tumour may develop in the same gland several years after the first has been removed and it occasionally undergoes malignant change.
Carcinoma
Malignant tumours most commonly affect the parotid glands. Some forms have a tendency to infiltrate nerves in the surrounding tissues, causing severe pain. Lymph spread is to the cervical nodes.
Diseases of the oesophagus
Learning outcomes
After studying this section, you should be able to:
explain how oesophageal varices develop
discuss the main inflammatory conditions of the oesophagus
describe the main oesophageal tumours
define oesophageal atresia and tracheo-oesophageal fistula.
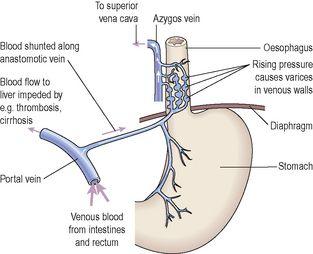
Oesophageal varices (
Fig. 12.46
)
In conditions such as cirrhosis (
p. 325
) or venous thrombosis, blood flow into the liver via the portal vein is impeded and blood pressure within the portal system rises (
portal hypertension
). This forces blood from the portal vein into anastomotic veins, which redirect (shunt) blood into the systemic venous circulation, bypassing the liver. Fifty per cent or more of the portal blood may be shunted into anastomotic veins, leading to rising pressure in these veins too. One route taken by the shunted blood is into veins of the distal oesophagus, which become distended and weakened by the abnormally high volume of blood.
Varices
(localised dilations of veins) develop when the weakest regions of the vessel wall bulge outwards into the lumen of the oesophagus, and, being thin walled and fragile, they are easily eroded or traumatised by swallowed food. Bleeding may be slight, but chronic, leading to iron deficiency anaemia (
p. 66
); however, sudden rupture can cause life-threatening haemorrhage.