Pediatric Examination and Board Review (182 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(A) a 4-year-old child with leukemia who develops fever and neutropenia
(B) a 20-year-old with an audible murmur diagnosed as mitral valve prolapse
(C) a 2-year-old child with a ventriculoperitoneal shunt secondary to hydrocephalus
(D) a 3-year-old child with a central venous catheter who is receiving total parenteral nutrition because of short bowel syndrome
(E) a 28-week premature neonate receiving total parenteral nutrition
11.
An 8-year-old girl has a fever of 103°F (39.4°C) for 2 days with cough, rhinorrhea, sore throat, and dyspnea. A chest radiograph reveals a small right lower lobe infiltrate. Antibiotic therapy with azithromycin is initiated, but 24 hours later, the child is evaluated at the emergency department. Findings on physical examination reveal an ill-appearing child, temperature: 104°F (40°C), respiratory rate 30/minute, blood pressure 60/25 mm Hg, hyperemic tonsils and posterior pharynx, and a generalized, erythematous, macular rash. A throat culture is obtained that reveals the colonies depicted in
Figure 103-1
. The most likely diagnosis is
(A) Stevens-Johnson syndrome
(B) Kawasaki disease
(C) Rocky Mountain spotted fever
(D) human monocytic ehrlichiosis
(E) streptococcal toxic shock syndrome
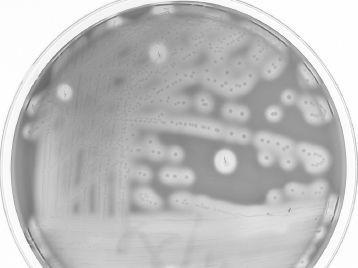
FIGURE 103-1.
Blood agar plate that reveals characteristic beta-hemolytic colonies characteristic of
S pyogenes
. Note the areas of enhanced beta-hemolysis where the agar was stabbed after the throat culture swab was plated.
12.
A pregnant woman is screened for rectal and vaginal colonization with group B streptococcus (GBS) at 35 weeks’ gestation. All of the following are indications for intrapartum prophylaxis to prevent early-onset GBS disease except
(A) GBS bacteriuria during current pregnancy
(B) delivery at 36 weeks’ gestation with unknown GBS status
(C) rupture of membranes for 18 hours during labor with unknown GBS status
(D) previous pregnancy with a positive GBS screening culture
(E) previous birth of infant with invasive GBS disease
13.
A 4-year-old girl has a high fever, and a blood culture is positive for
E faecalis
. In which clinical setting is enterococcal bacteremia most likely to occur with this young girl?
(A) child hospitalized in the pediatric intensive care unit with a central venous catheter
(B) child with first episode of a urinary tract infection
(C) child with a seizure and a lumbar puncture revealing CSF pleocytosis
(D) child with an isolated ventricular septal defect
(E) newborn infant born to a mother with chorioamnionitis
14.
A 15-year-old adolescent girl develops pain in the hands and wrists 4 days after the start of her menstrual period. She then develops scattered papules on both hands while the pain in the hands and wrists improves. She then develops swelling of her left knee, which prompts medical attention. You suspect disseminated gonococcal infection. The most reliable method to diagnose this infection is by
(A) culture of blood
(B) PCR of blood
(C) culture of joint fluid
(D) gram stain smear of pharyngeal secretions
(E) culture or rRNA probe of endocervical secretions
15.
A 3-year-old boy is bitten on his right lower leg by a dog in the neighborhood. Twelve hours later he develops fever to 102°F (38.8°C) and chills. The bite wound has swelling, erythema, tenderness, and a serosanguineous drainage. The most likely etiology of this wound infection is
(A)
Eikenella corrodens
(B)
Pasteurella multocida
(C)
P aeruginosa
(D)
S pyogenes
(E)
Salmonella
serotype
Marina
16.
A 4-year-old girl develops fever, vomiting, and hematochezia. A stool culture grows
Salmonella enteritidis
. The child recovers from the illness, but a stool culture sent 12 weeks later is still positive for
S enteritidis
. The organism is susceptible to ampicillin, ceftriaxone, trimethoprim-sulfamethoxazole, and gentamicin. At this point appropriate treatment would include
(A) trimethoprim-sulfamethoxazole
(B) gentamicin
(C) high-dose amoxicillin combined with probenecid
(D) no antimicrobial therapy
(E) cefixime
17.
A 3-year-old girl develops fever, abdominal cramps, and mucoid bloody stools. A stool culture grows
S sonnei
, and the child is treated with trimethoprimsulfamethoxazole based on susceptibility testing. Two days after the onset of the girl’s symptoms, her 2-year-old brother also develops fever, vomiting, and profuse watery diarrhea. A stool culture is negative. Appropriate management of this sibling includes
(A) antimicrobial therapy with trimethoprimsulfamethoxazole
(B) diagnostic assay of stool for rotavirus antigen
(C)
C difficile
toxin assay on stool
(D) CBC with differential
(E) repeat stool culture for
S sonnei
18.
In December, a 6-month-old male infant develops fever, vomiting, and diarrhea that contains mucus and blood. He is bottle-fed infant formula. A stool culture sent grows
Yersinia enterocolitica
. The most likely source of the
Y enterocolitica
in this case is
(A) contaminated well water
(B) pork intestines (chitterlings)
(C) pasteurized milk
(D) raspberry-flavored baby food
(E) contaminated apple juice
ANSWERS
1.
(A)
Although all of the bacterial pathogens listed can cause pneumonia with empyema,
S aureus
is the most common cause among these pathogens.
S pneumoniae
is another major cause, but the child has been immunized. Use of the pneumococcal conjugate vaccine has resulted in a decrease in the incidence of invasive pneumococcal disease, including pneumonia/empyema.
2.
(A)
Clindamycin would be the most appropriate antibiotic in this case of community-associated MRSA infection after surgical drainage. There has been an increase in soft tissue infections as well as more serious invasive infections because of MRSA in most areas of the United States. Vancomycin should be reserved for more critically ill patients.
3.
(C)
Botulism is caused by
Clostridium botulinum
, a gram-positive anaerobic bacillus found in soil and agricultural products. Ingestion of honey is a risk factor for infant botulism, but in most infants, no source of the
C botulinum
spores can be found. Decreased frequency of bowel movements is a common symptom as are the other clinical features listed. The diagnosis can be confirmed by culture of the organism or identification of
C botulinum
toxin in the stool. The mainstay of management of infants with botulism is supportive care. Human botulism immune globulin intravenous (BIG-IV) is available for treatment.
4.
(C)
The initial goals of treatment of tetanus include neutralization of toxin, eradication of
C tetani,
and supportive care. Antimicrobial therapy to eradicate the organism can include metronidazole, penicillin, or tetracycline. IVIG can be considered for treatment if TIG is not available. Tetanus toxoid will not provide antibody quickly enough to be helpful.
5.
(B)
Listeria monocytogenes
can manifest a similar clinical picture to that caused by
Streptococcus agalactiae
(group B streptococcus) with early-onset sepsis or late-onset meningitis. Prematurity, pneumonia, and septicemia are common in early-onset disease. Perinatal infection can result in stillbirth or neonatal death in approximately 20% of infections in pregnancy.
6.
(C)
There was been an increase in reported cases from 1997 to 2009 of pertussis in adolescents and adults. Up to a third of adolescents and adults with prolonged cough illness were shown to have pertussis. Neonates with pertussis are likely to have been born to young mothers with an illness characterized by cough. These findings support the current concept that older individuals are the major reservoirs of
B pertussis
. Conjunctivitis is not a feature of pertussis, but post-tussive emesis is. Nearly 17,000 cases were reported in 2009.
7.
(B)
The Gram stain that reveals gram-negative coccobacilli is consistent with
H influenzae
. The incidence of
H influenzae
type b meningitis has declined dramatically since routine immunization of young infants against
H influenzae
type b began. Invasive disease by non–type b encapsulated strains and nontypeable strains still does occur, and in most states, the incidence of invasive disease due to non–type b strains is higher than with type b strains. A recent vaccine shortage was announced with a small uptick of serotype b illness that was rare among fully immunized children.
8.
(A)
Amoxicillin is the drug of choice for treatment of acute otitis media, including infection caused by penicillin-nonsusceptible
S pneumoniae
. With use of this dose of amoxicillin, the concentration of the antibiotic in middle ear fluid is believed to be high enough to eradicate penicillin nonsusceptible strains of
S pneumoniae
. The addition of clavulanate unnecessarily broadens the antimicrobial spectrum.
9.
(C)
Chemoprophylaxis to prevent invasive meningococcal disease for health-care professionals is not recommended unless there is intimate exposure to a patient with invasive meningococcal disease because a measurable attack rate has not been documented among such personnel. This type of exposure would include unprotected mouth-to-mouth resuscitation, intubation, or suctioning of the patient before antimicrobial therapy was administered.
10.
(C)
Most coagulase-negative staphylococci (CoNS) isolated from blood cultures are common inhabitants of the skin and mucous membranes and are procedural contaminants of blood culture techniques. Risk factors for actual CoNS infection would include catheter placement, medical device insertion, or immunosuppression. CoNS are common causes of ventriculoperitoneal shunt infections, but secondary bacteremia or bacteremic seeding of the shunt does not occur. CoNS may also cause urinary tract infections, particularly in adolescent girls and young adult women. The species involved is most commonly
S saprophyticus
. Children with fever and neutropenia who have CoNS bacteremia most often have central venous catheters in place.
11.
(E)
Toxic shock syndrome (TSS) can be caused by toxin-producing
S aureus
or
S pyogenes
stains. In children a major risk factor for streptococcal TSS is concomitant varicella. Both etiologies of TSS can occur without an identifiable focus of infection (
Table 103-1
).
