Oxford Handbook of Midwifery (99 page)
Read Oxford Handbook of Midwifery Online
Authors: Janet Medforth,Sue Battersby,Maggie Evans,Beverley Marsh,Angela Walker

- Call medical aid.
- Explain the situation to the mother.
- Carry out a vaginal examination.
- If an oxytocic infusion is running, this should be stopped immediately.
- Relieve pressure on the umbilical cord by keeping your fingers in the vagina to push the presenting part away from the umbilical cord.
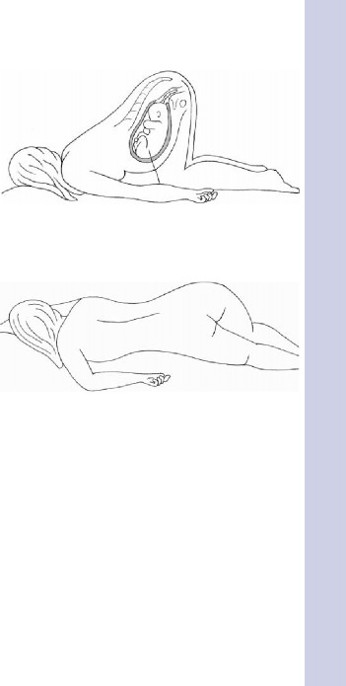
- Assist the woman to move into the knee-chest position, which helps to relieve compression of the umbilical cord (Fig. 19.3). Alternatively, the exaggerated Sim’s position (Fig. 19.4) may be adopted, by lying her on her side with a wedge or pillow to raise her hips. The foot of the bed can be elevated.
- Monitor the FHR.
- Urgent delivery.
- In some units alternative management may involve displacing the presenting part by filling the bladder with 500mL of normal saline. The catheter is then clamped and the fingers may then be withdrawn from the vagina. The clamp is released when the incision for LSCS is being made and therefore delivery is imminent.
Cord presentation
- Will usually have been diagnosed on vaginal examination.
- May be associated with deceleration of the FHR.
- Do
not
rupture the membranes. - Discontinue the vaginal examination.
- Call for medical assistance.
- Monitor the FHR.
- Encourage the woman to adopt a position as above that will reduce the occurrence of cord compression.
- Expedite delivery as soon as possible—LSCS is the most likely outcome.
Cord presentation and cord prolapse constitute a serious threat to fetal well-being. In order to reduce mortality and morbidity, it is important that urgent delivery is initiated. This will usually be by caesarean section if the fetus is alive and delivery is not imminent. In some instances, with a multiparous woman, a second-stage vaginal delivery may be possible. In the community, where the fetus is alive, arrange urgent transfer to hospital.
CORD PRESENTATION AND CORD PROLAPSE
443
Fig. 19.3
Knee chest position (relieves compression on prolapsed cord).Fig. 19.4
Sim’s position.
CHAPTER 19
Emergencies444
Vasa praevia
- This is a rare occurrence when a fetal blood vessel is situated over the cervical os and therefore is in front of the presenting part.
- There may be a velamentous insertion of the cord (or possibly a succenturiate lobe) resulting in a fetal vessel running through the membranes.
Diagnosis
- The presence of the vessel might be suspected during vaginal examination while the membranes are still intact.
- If a careful speculum examination were performed with a good light it might be possible to see the vessel.
Rupture of the vessel
- This may occur if the membranes rupture.
- The fetus may die unless quickly delivered.
Signs and symptoms
- Minimal fresh red loss occurring typically at the rupture of the membranes.
- On monitoring the fetal heart there are signs of fetal compromise which are disproportionate to the amount of blood loss.
- There may be a sinusoidal fetal heart pattern sometimes seen when the fetus is severely anaemic. This is characterized by increased variability of >15 beats and resembles a sine wave with 2–6 cycles per min.
Immediate care
The midwife should:
- Recognize the risk of fetal asphyxia (b see Hypoxia and asphyxia, p. 434).
- Call for help speedily from the obstetric registrar and team.
- Continue to record a CTG.
- If the fetal compromise is apparent prepare the woman for very urgent caesarean section (b see Emergency LSCS, p. 379) if this is the first stage of labour.
- If delivery is imminent or the woman is multiparous in the second stage of labour encourage pushing or/and if requested prepare for forceps/ ventouse delivery.
- The paediatrician should be called to the delivery.
- The cord should be double clamped and blood should be obtained for blood gases and also for haemoglobin estimation in the baby.
- The paediatric team will transfer the baby to SCBU for observation and treatment. S/he may require a blood transfusion.
This page intentionally left blank
CHAPTER 19
Emergencies446
Shoulder dystocia
Definition
Impaction of the anterior shoulder behind the symphysis pubis, which impedes the spontaneous delivery of the baby.
Incidence
- 0.15–2% of all vaginal deliveries.
- Although this is a relatively rare event, the perinatal mortality can be between 2.6% and 29%, with surviving babies at risk of long-term morbidity.
- The Confidential Enquiry into Stillbirths and Deaths in Infancy (CESDI) (1996)
1
report recommended that all professionals involved with delivery of a baby must be trained to deal with this emergency. - This is one of the most frightening emergencies experienced, as it is difficult to predict and the midwife facilitating the birth may be working alone.
Predisposing factors
- Maternal obesity
- Maternal diabetes
- Post dates, >41 weeks
- Previous shoulder dystocia or big baby
- Macrosomia in present pregnancy
- Prolonged first and/or second stage of labour
- Operative delivery, especially mid-cavity instrumental delivery for delay.
The predisposing factors may not be present in every case, so the first sign is often failure of the baby’s chin to escape the perineum, or failure of the baby’s head to undergo restitution or rotation. This is sometimes referred to as the ‘turtle’ sign. The baby’s head is pressing so tightly against the perineum that it is impossible to insert a finger into the vagina, and the baby’s face becomes suffused and discoloured.
The following mnemonic, HELPER, is adapted from the Advanced Life Support in Obstetrics:
- H = HELP, call for help: obstetrician, anaesthetist, midwives, paediatric team, and support workers.
- NOTE THE TIME OF THE DELIVERY OF THE HEAD
- E = EVALUATE for EPISIOTOMY, episiotomy scissors open, symphysiotomy tray available.
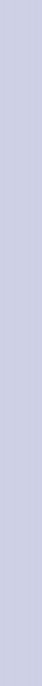
- L = LEGS, lay the bed flat, remove pillows, lift the woman’s knees to her shoulders (McRobert’s position, see Fig. 19.5).
- P = PRESSURE: SUPRAPUBIC, constant for 30s, direct the baby’s shoulder towards his or her chest, rocking pressure for 30s (see Fig. 19.6).
- E = ENTER PELVIS
- Episiotomy.
- Pressure on posterior aspect of the baby’s anterior shoulder, try to get baby’s shoulders into oblique diameter.

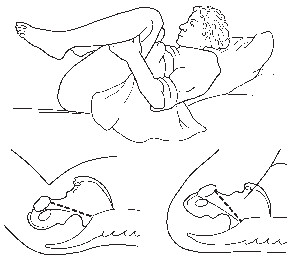
Fig. 19.5
McRobert’s manoeuvre.Reprinted by permission of Henry Lerner M.D. from M www.shoulderdystociainfo.com
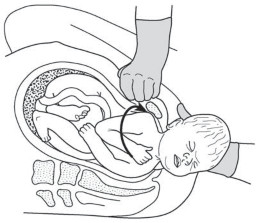
Fig. 19.6
Suprapubic pressure, divert the baby’s shoulder towards his chest.Reprinted by permission of Henry Lerner M.D. from M
www.shoulderdystociainfo.com.SHOULDER DYSTOCIA
447
CHAPTER 19
Emergencies448
- Continue pressure and rotate the baby by 180° (the baby’s anterior shoulder now be posterior) (Fig. 19.7).
- Pressure on the posterior aspect of the baby’s posterior shoulder, try to get baby’s shoulders into oblique diameter.
- Continue pressure and rotate the baby by 180° (the baby’s posterior shoulder becomes anterior) (Fig. 19.8).
- Episiotomy.
- Call medical aid.
Other books
An Uncertain Affair (The Affair Series Book 2) by Randi Ocean
Remedy Z: Solo by Dan Yaeger
Stonebound: Shifters Forever Worlds (Skeleton Key) by Elle Thorne, Skeleton Key
Blood Sweep by Steven F Havill
Mundahlia (The Mundahlian Era, #1) by RJ Gonzales
On Deadly Ground by Lauren Nichols
CARNAL APPETITE by Celeste Anwar
The Godlost Land by Curtis, Greg
Rise of a Legend (Guardian of Scotland Book 1) by Amy Jarecki
Detroit Rock City by Steve Miller
