i bc27f85be50b71b1 (56 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown


180 Aurn CARt- IIANDBOOK H)R I'II),\I<"AI IIUR:\IlI\P ..
from a stumbling fall.' Patellar fractures arc associated with ipsilateral
distal femoral or shaft fractures, proximal tibial condyle fractures, and
posterior dislocation of the hip." Late complications include patel·
lofemoral or hardware pain, osteoarthritis, and decreased terminal
extension from abnormal patellar mechanics, quadriceps weakness, or
adhesions. Chapter Appendix Table 3-A.7 describes the management
of patellar fractures. Most orthopedic surgeons perform partial or
total patellectomy as a last resort because of the high incidence of an
impaired quadriceps mechanism months latcr.l!
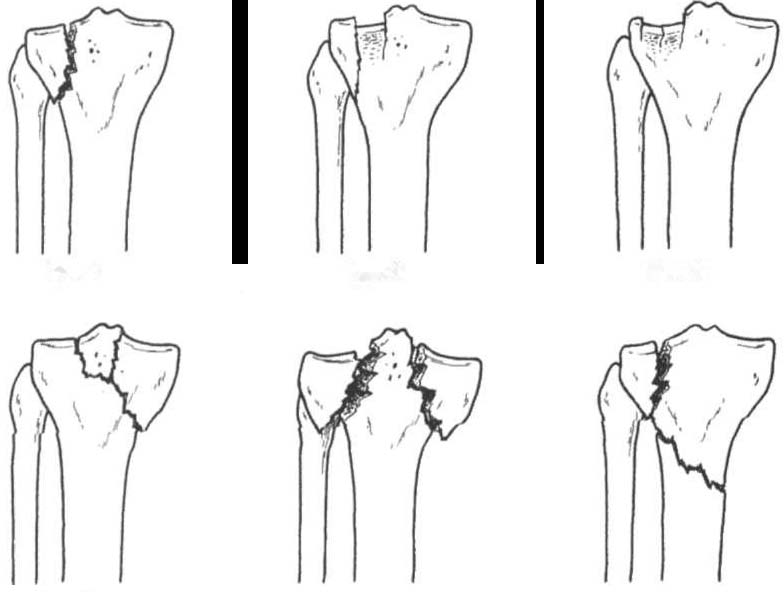
Tibial Plateau Fraclllre
Tibial plateau fractures result from direct force on the proximal tibia
(e.g., when a pedestrian is hit by an automobile), as shown by the Schatzker classification in Figure 3-7. This high-force InJury often presents with open wounds, soft tissue injuries, ligamentous disruption, and dislocation. Contralateral collateral ligament injuries occur from varus or valgus force of injury.7 Ligamentous injuries are most common in nondisplaced,
compressed, and split compression fractures.I1
The complexity of tibial plateau fractures cannot be overstated.
Chapter Appendix Table 3-A.8 lists the management of tibial plateau
fractures. fmmediate or early complications of tibial plateau fractures
include popliteal or peroneal nerve compression, compartment syndrome, infection, and DVT. Late complications Include abnormal patellofemoral mechanics, lack of ROM or stability, and post-traumatic arthritis of the articular surface.
Tibial Shaft alld Fibula Fractures
Tibial shaft and fibula fractures result from lugh-energy trauma (e.g.,
MVAs, crush injuries, skiing accidents) via direct blow, twisting of the
ankle, or varus stress on the knee.' The higher the energy on impact, the
morc soft tissue and bone damage occurs. Tibial shaft fracture management (Chapter Appendix Table 3-A.9) is very complicated because of associated injuries similar to those of tibial plateau fractures. Immediate
or early complications include anterior tibial artery damage, interosseous
membrane rupture, peroneal nerve injury, or degloving injuries. Delayed
or late complications include malunion, nonunion, osteomyelitis, secondary amputation, or reflex sympathetic dysrrophy. The distal lower extremity must be thoroughly evaluated for concomitant ankle trauma (e.g., trimalleolar fracture, syndesmotic disruption, or talar dome fracture).
Distal Tibial and Ankle fraclures
Fractures of the distal tibia, distal fibula, and talus are described
togerher because of their frequent simultaneous injury. Distal tibial
MUSCULOSKELETAL SYSTEM 181
Type 1
Type 2
Type 3
Type 4
Type 5
TypeS
Figure 3-7. Classification of (ibial plateau (ractures (Schatzker). Type 1
wedge (racture of the lateral tibial plateau. Type 2 wedge (rac/ure of the lat·
eral plateau with depression of the adiacellt pla/eall. Type 3 central depressiOtz of the articular surface of the lateral plateau without a wedge fragment.
Type 4 {racture of the medial tibial plateau. Type 5 bicondylar (racture. Type
6 tibial plateau (racture with separation of metaphysis from diaphysis. (With
permission from A Unwin, K JONes !eds/. Emergency Orthopaedics and
Trauma. Boston: Buuerworth-Heinemaml, 1995;226.)
fractures (i.e., pilon fractures) are the result of high vertical loading
forces, such as with parachuring accidents, falls from heights, sporting injuries, and MVAs.23 Often, long axis compression throughout the proximal lower extremity can cause associated tibial plateau fracture, hip dislocation, or acetabular fracture.
Ankle fractures commonly result from torque caused by abnormal
loading of the talocrural joint with body weight. Fractures may be
simple, involving avulsion of a portion of the distal fibula, or complex, involving rhe enrire morrise (trimalleolar fracture) with disruption of the syndesmosis. Fracture severity depends on the degree of foot inversion or eversion in relation to the subtaiar joint ar the time
of injury.23 Stability of the ankle depends on joint congruity and ligamentous inregrity. Complications associated with ankle fractures arc

182 AClITE CARE HANDBOOK FOR PHYSICAL THERAPISTS
malunion, delayed union, traumatic arthritis, and osteomyelitis.21
Chapter Appendix Table 3-A.IO lists distal tibial and ankle fracture
management.
Calcalleal alld Forefoot Fractures
The mosr commonly fractured bone of the foot is the calcaneus, with
fractures caused by a direct blow, such as a fall from a height or as an
avulsion injury from a strong contraction of the triceps surae. Calcaneal fractures, usually bilateral, are associated with additional proximal leg injury or spinal fracture (e.g., burst fracture)." Latent complications of complex calcaneal fracture include joinr pain, peroneal tendonitis, and heel spur from malunion.24
Forefoot fracture or metatarsal fracture occurs as a crush injury
when a heavy object lands on the foot, as a rwisting injury, as a suess
fracture, or as an avulsion fracture at the base of the fifth metatarsal
from forceful peroneus brevis contraction? Chapter Appendix Table
3-A.ll lists the general types and management of calcaneal and forefoot fractures.
Spine
In order of frequency, fractures of the spine are caused by automobile
or motorcycle accidents, falls, sports accidents, and violence as a
result of flexion, extension, roration, and vertical compression
forces.25 Spinal fracture at any level is discussed in terms of location
(anterior or posterior column) or stability (mechanical or neurologic).
Anatomically, the anterior column refers to the vertebral bodies and
intervertebral discs including the anterior and posterior longitudinal
ligaments.25 The posterior column refers to the transverse and spinous
processes, pedicles, laminae, and facets, including the interspinous,
infraspinous, supraspinous, and nuchal ligaments.25
A fracture may be considered stable if there is disruption of either
the anterior or posterior column or an injury without neurologic compromise. An unstable fracture occurs if both the anterior and posterior columns are disrupted or if there is a potential for neurologic compromise. Potential neurologic injury can occur from progressive
swelling at the site of the injury, hematoma formation, and associated
intervertebral disc herniation or dislocation. Spinal fracture may
occur with or without spinal cord injury (refer to Spinal Cord Injury
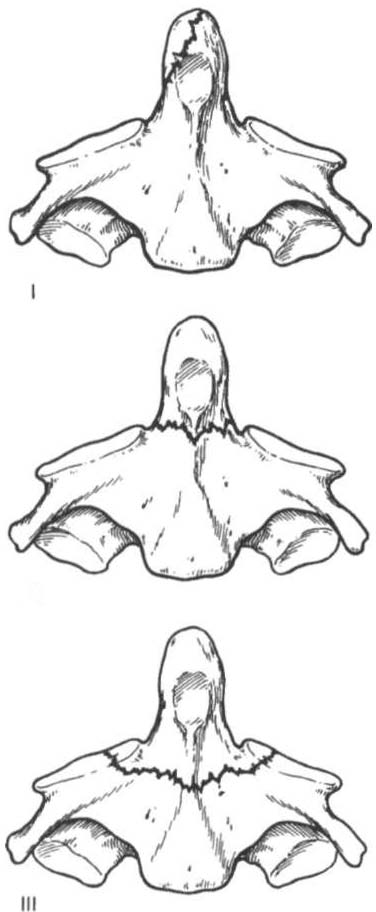
in Chapter 4). Figures 3-8 and 3-9 are examples of high cervical
(odontoid) and lumbar burst fractures.
Basic cervical and thoracolumbar fracture description and management are described in Chapter Appendix Table 3-A. J 2 and 3-A.13,