The Coming Plague (140 page)
Authors: Laurie Garrett

150
K. Brudney and J. Dobkin, “Resurgent Tuberculosis in New York City,”
American Review of Respiratory Disease
144 (1991): 745â49.
American Review of Respiratory Disease
144 (1991): 745â49.
151
C. Woodard, “TB in New York,”
New York Newsday
, March 8, 1992: 1; C. Woodard, “Bitter Medicine to Swallow,”
New York Newsday
, March 8, 1992: 38; M. Gelman, “A Prison Breeding Ground,”
New York Newsday,
March 11, 1992: 23; M. Gelman, “City Races to Finish âCutting Edge' TB Jail,”
New York Newsday
, March 11, 1992: 87; L. Garrett and C. Woodard, “New Risk in Hospitals,” New
York Newsday
, March 10, 1992: 6; L. Garrett, “HIV/TBâTandem Epidemics Breed a Contradiction in Control,”
New York Newsday
, March 31, 1992: 57; L. Garrett, “Jobs That Carry a High Risk of TB,”
New York Newsday
, March 31, 1992: 61; L. Garrett, “Tackling the TB Puzzle,”
New York Newsday
, March 12, 1992: 8; and G. Cowley, E. A. Leonard, and M. Hager, “A Deadly Return,”
Newsweek
, March 16, 1992: 53â57.
New York Newsday
, March 8, 1992: 1; C. Woodard, “Bitter Medicine to Swallow,”
New York Newsday
, March 8, 1992: 38; M. Gelman, “A Prison Breeding Ground,”
New York Newsday,
March 11, 1992: 23; M. Gelman, “City Races to Finish âCutting Edge' TB Jail,”
New York Newsday
, March 11, 1992: 87; L. Garrett and C. Woodard, “New Risk in Hospitals,” New
York Newsday
, March 10, 1992: 6; L. Garrett, “HIV/TBâTandem Epidemics Breed a Contradiction in Control,”
New York Newsday
, March 31, 1992: 57; L. Garrett, “Jobs That Carry a High Risk of TB,”
New York Newsday
, March 31, 1992: 61; L. Garrett, “Tackling the TB Puzzle,”
New York Newsday
, March 12, 1992: 8; and G. Cowley, E. A. Leonard, and M. Hager, “A Deadly Return,”
Newsweek
, March 16, 1992: 53â57.
152
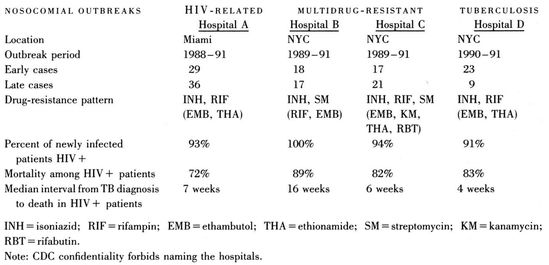
Source: Centers for Disease Control.
153
D. E. Snider and W. L. Roper, “The New Tuberculosis,”
New England Journal of Medicine
325 (1992): 703â5; F. Gordin, “Tuberculosis ControlâBack to the Future?”
Journal of the American Medical Association
267 (1992): 2649â50; P. F. Barnes, A. B. Bloch, P. T. Davidson, and D. E. Snider, “Tuberculosis in Patients with Human Immunodeficiency Virus Infection,”
New England Journal of Medicine
324 (1991): 1644â50; and M. A. Fischl, G. L. Daikos, R. B. Uttamchandani, et al., “Clinical Presentation and Outcome of Patients with HIV Infection and Tuberculosis Caused by Multiply-Drug-Resistant Bacilli,”
Annals of Internal Medicine
117 (1992): 184â90.
New England Journal of Medicine
325 (1992): 703â5; F. Gordin, “Tuberculosis ControlâBack to the Future?”
Journal of the American Medical Association
267 (1992): 2649â50; P. F. Barnes, A. B. Bloch, P. T. Davidson, and D. E. Snider, “Tuberculosis in Patients with Human Immunodeficiency Virus Infection,”
New England Journal of Medicine
324 (1991): 1644â50; and M. A. Fischl, G. L. Daikos, R. B. Uttamchandani, et al., “Clinical Presentation and Outcome of Patients with HIV Infection and Tuberculosis Caused by Multiply-Drug-Resistant Bacilli,”
Annals of Internal Medicine
117 (1992): 184â90.
154
Centers for Disease Control, “Drug-Resistant Tuberculosis Among the HomelessâBoston,”
Morbidity and Mortality Weekly Report
34 (1985): 429â31.
Morbidity and Mortality Weekly Report
34 (1985): 429â31.
155
Centers for Disease Control, “Multi-Drug-Resistant TuberculosisâNorth Carolina,”
Morbidity and Mortality Weekly Report
35 (1987): 785â87.
Morbidity and Mortality Weekly Report
35 (1987): 785â87.
156
For these and other chilling findings, see a lengthy memo from the CDC to the Department of Health and Human Services, Washington, D.C., dated December 31, 1991; and T. R. Frieden, M. L. Pearson, and J. A. Jereb, “Drug Resistant and Nosocomial Tuberculosis, New York City, 1991,”
EPI-AID
(1991): EPI-91-42â2.
EPI-AID
(1991): EPI-91-42â2.
157
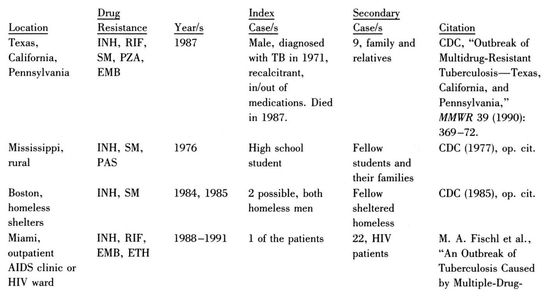
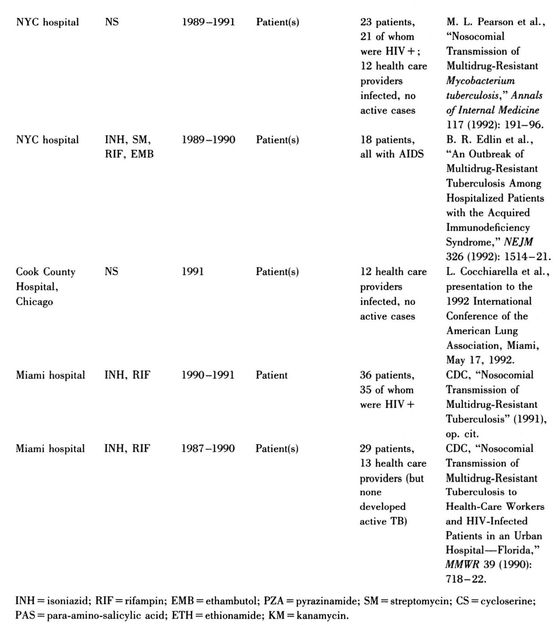
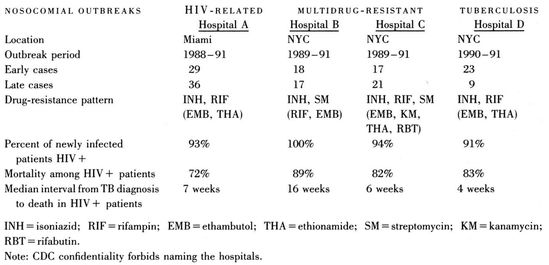
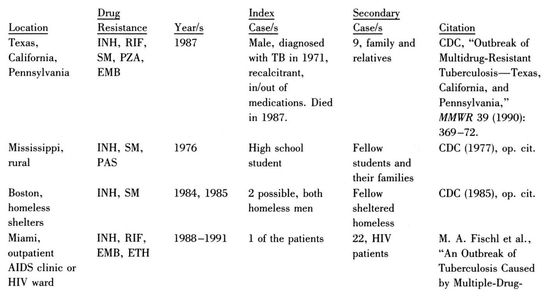
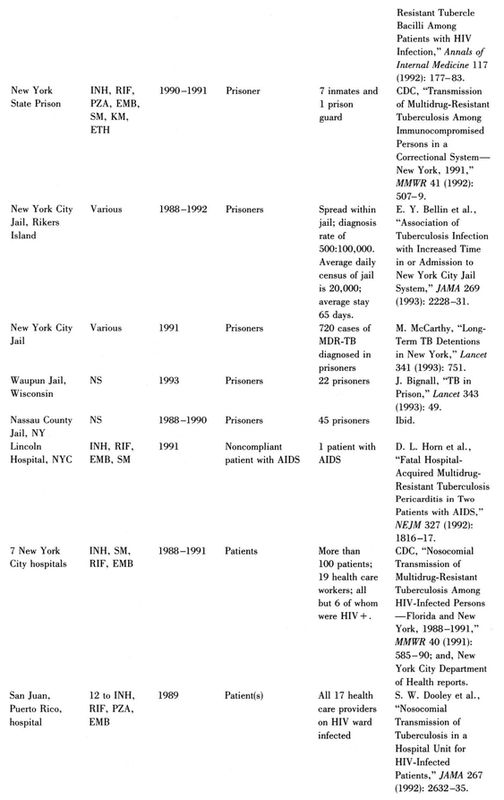
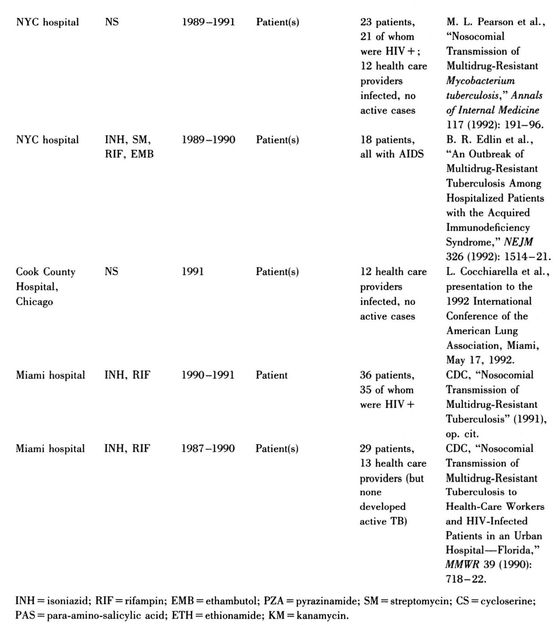
There were many outbreaks of MDR-TB in the United States and Puerto Rico during the epidemic, which appears to have begun sometime in the mid-1980s and continues at this writing.
Â
MDR-TB OUTBREAKS REPORTED IN THE UNITED STATES AND PUERTO RICO, 1985â92
158
R. E. Brown, C. S. Palmer, and K. Simpson, “Estimate of Identifiable Costs of Tuberculosis in the United States in 1991,” Battelle Medical Technology Assessment and Policy Research Center, Washington, D.C., 1993.
159
New York State Assembly Committee on Health, “Tuberculosis in New York: The Return of an Epidemic,” Report to the Legislature, Albany, 1991.
160
The actual allocation approved by the White House was for $40 million in 1992. CDC director Roper “found” another $14.9 million in funds designated for AIDS education efforts. Of the total $54.9 million, $6.5 million went to the National Institutes of Health for basic TB research and $46.5 million went to CDC tuberculosis control. Of its share, the CDC sent a good portion to New York City.
Already facing a budget crisis, New York City spent more than $40 million on TB control in 1992 alone.
The NIH's TB spending climbed from $3.5 million in 1991 to $46 million in 1994.
161
The cities surveyed were Atlanta, Baltimore, Boston, Chicago, Cleveland, Dallas, Detroit, Honolulu, Jacksonville, Los Angeles, Memphis, Miami, Milwaukee, Nashville, Newark, New Orleans, New York, Philadelphia, Phoenix, San Antonio, San Diego, San Francisco, Seattle, Tampa, and Washington, D.C. See D. R. Leff and A. R. Leff, “Tuberculosis Control Policies in Major Metropolitan Health Departments in the United States: V. Standard of Practice in 1992,”
American Reviews of Respiratory Disease
148 (1993): 1530â36.
American Reviews of Respiratory Disease
148 (1993): 1530â36.
162
Tuberculosis Task Force, “Nassau County Policy Plan for Responding to the Metropolitan New York Tuberculosis Epidemic,” Report to the Nassau County Health Department, November 1993.
163
M. Goble, M. D. Iseman, L. A. Madsen, et al., “Treatment of 171 Patients with Pulmonary Tuberculosis Resistant to Isoniazid and Rifampin,”
New England Journal of Medicine
328 (1993): 527â32.
New England Journal of Medicine
328 (1993): 527â32.
164
D. E. Snider, “Shortages of Antituberculosis Drugs, Outbreaks of Multidrug-Resistant Disease and New Drug Development in the U.S.,” presentation to the World Health Organization, November 22, 1991.
165
New York City Task Force on Tuberculosis in the Criminal Justice System, “Final Report to Mayor David N. Dinkins and Margaret A. Hamburg, M.D., Commissioner, Department of Health,” June 1992.
166
Among the questions TB scientists at the February 10, 1992, meeting identified as most pressing were the following:
Epidemiology
⢠How long do the bacteria survive in an enclosed airspace, potentially infecting a person?
⢠How many bacteria does a human need to be exposed to in order to be infected?
⢠What, precisely, are the relationships between HIV, injecting drug use, poverty, poor housing, and tuberculosis?
Treatment
⢠How can laboratories shorten the amount of time required to diagnose MDR-TB to some clinically useful period?
⢠What are the optimal ways to use antitubercular drugs to avoid development of resistance?
⢠What are the risks for patient reinfection?
⢠What steps should hospitals and individual health providers take to avoid catching TB from their patients? To prevent patient-to-patient transmission?
⢠How can surfaces be sterilized for TB?
⢠Are there any other drugs out there for TB?
⢠Can anything be done to save HIV-positive people who become infected with MDR-TB?
Pathogenesis/Immunology
⢠How does the bacteria use complement receptors to gain entry into human cells?
⢠Why do the bacteria have strong iron-binding capabilities?
⢠What is the nature of the cell-mediated immune response to the microbe? Do antibodies play any significant role?
⢠How much of the disease is due to macrophages' release of cytokines and other chemicals following
M. tuberculosis
invasion?
M. tuberculosis
invasion?
⢠Why does the human lung self-destruct when infected?
⢠How do the bacterial colonies form the protective encasements that allow them to hide from the immune system? And what, exactly, causes the liquefaction process that melts those casings and floods the bloodstream with the bacteria?
⢠Are any of the bovine-based BCG vaccines against TB useful? How useful? For whom?
Resistance
Resistance
⢠What is the molecular/genetic basis of drug resistance? Does it always vary from drug to drug, or are there universal resistance mechanisms?
⢠Is there any way to design a drug that the mycobacteria can't resist?
167
Y. Zhang, B. Heym, B. Allen, et al., “The Catalase-Peroxidase Gene and Isoniazid Resistance of
Mycobacterium tuberculosis
,”
Nature
358 (1992): 591â92; and A. Banerjee, E. Dubnau, A. Quemard, et al., “InhA, a Gene Encoding a Target for Isoniazid and Ethionamide in
Mycobacterium tuberculosis
,”
Science
263 (1993): 227â30.
Mycobacterium tuberculosis
,”
Nature
358 (1992): 591â92; and A. Banerjee, E. Dubnau, A. Quemard, et al., “InhA, a Gene Encoding a Target for Isoniazid and Ethionamide in
Mycobacterium tuberculosis
,”
Science
263 (1993): 227â30.
168
B. J. Culliton, “Drug-Resistant TB May Bring Epidemic,”
Nature
356 (1992): 473.
Nature
356 (1992): 473.
169
W. R. Jacobs, R. G. Barletta, R. Udani, et al., “Rapid Assessment of Drug Susceptibilities of
Mycobacterium tuberculosis
by Means of Luciferase Reporter Phages,”
Science
260 (1993): 819â22.
Mycobacterium tuberculosis
by Means of Luciferase Reporter Phages,”
Science
260 (1993): 819â22.
170
P. Pancholi, A. Mirza, N. Bhardwaj, and R. M. Steinman, “Sequestration from Immune CD4+ T Cells of Mycobacteria Growing in Human Macrophages,”
Science
260 (1993): 984â86; and S. Arruda, G. Bomfim, R. Knights, et al., “Cloning of a
Mycobacterium tuberculosis
DNA Fragment Associated with Entry and Survival Inside Cells,”
Science
261 (1993): 1454â58.
Science
260 (1993): 984â86; and S. Arruda, G. Bomfim, R. Knights, et al., “Cloning of a
Mycobacterium tuberculosis
DNA Fragment Associated with Entry and Survival Inside Cells,”
Science
261 (1993): 1454â58.
171
Somewhat after the emergence of MDR-TB in the United States, European communities of poverty witnessed identical chains of social and biological events. In Switzerland, the Netherlands, Italy, Denmarkâall over EuropeâHIV, poverty, and injecting drug use drove tuberculosis rates upward. According to WHO, Western Europe's increases were as follows:
| Country | Time Period | Percent Increase in TB |
|---|---|---|
| Switzerland | 1986â90 | 33 |
| Denmark | 1984â90 | 31 |
| Italy | 1988â90 | 28 |
| Norway | 1988â91 | 21 |
| Ireland | 1988â90 | 18 |
| Austria | 1988â90 | 17 |
| Finland | 1988â90 | 17 |
| Netherlands | 1987â90 | 9.5 |
| Sweden | 1988â90 | 4.6 |
| United Kingdom | 1987â90 | 2.0 |
| France, Germany, Belgium | 1987â91 | stable |
Source: World Health Organization, Press Release, June 17, 1992.
See also A. Genewein, A. Telenti, C. Bernasconi, et al., “Molecular Approach to Identifying Route of Transmission of Tuberculosis in the Community,”
Lancet
342 (1993): 841â44; and E. Drucker, “Molecular Epidemiology Meets the Fourth World,”
Lancet
342 (1993): 817â18.
Lancet
342 (1993): 841â44; and E. Drucker, “Molecular Epidemiology Meets the Fourth World,”
Lancet
342 (1993): 817â18.
172
K. Brudney and J. Dobkin, “A Tale of Two Cities: Tuberculosis Control in Nicaragua and New York City,” unpublished, 1992.
173
D. Wilkinson, “High-Compliance Tuberculosis Treatment Programme in a Rural Community,”
Lancet
173 (1994): 647â48.
Lancet
173 (1994): 647â48.
174
E. P. Y. Muhondwa, “The Role and Impact of Foreign Aid in Tanzania's Health Development,” in M. R. Reich and E. Marvi, eds.,
International Cooperation for Health: Problems, Prospects, and Priorities
(Dover, MA: Auburn House, 1989).
International Cooperation for Health: Problems, Prospects, and Priorities
(Dover, MA: Auburn House, 1989).
175
C. Murray, K. Styblo, and A. Rouillon, “Tuberculosis,” in D. T. Jamison and W. H. Mosley, eds.,
Disease Control Priorities in Developing Countries
(New York: Oxford University Press, 1991).
Disease Control Priorities in Developing Countries
(New York: Oxford University Press, 1991).
176
Sadly, the U.S. Agency for International Development cut its entire overseas tuberculosis budgetâall $3 millionâthe day after Christmas 1993. That represented a third of all funds for the World Health Organization's TB program.
177
Some countries had no tuberculosis control program at all. There, of course, the TB situation could have been worse than in the United States. The World Bank chose to limit comparisons to countries with TB programs and prevalence data.
178
In 1994, the CDC and the New York City Department of Health cautiously announced some success in DOT control of TB, but repeatedly warned physicians and the general public not to misinterpret their findings as indicating that the epidemic was under control. See A. B. Bloch, G. M. Cauthen, I. Onorato, et al., “Nationwide Survey of Drug-Resistant Tuberculosis in the United States,”
Journal of the American Medical Association
271 (1994): 665â71; and S. E. Weis, P. C. Slocum, F. X. Blais, et al., “The Effect of Directly Observed Therapy on the Rates of Drug Resistance and Relapse in Tuberculosis,”
New England Journal of Medicine
330 (1994): 1179â84.
Journal of the American Medical Association
271 (1994): 665â71; and S. E. Weis, P. C. Slocum, F. X. Blais, et al., “The Effect of Directly Observed Therapy on the Rates of Drug Resistance and Relapse in Tuberculosis,”
New England Journal of Medicine
330 (1994): 1179â84.
179
National MDR-TB Task Force, “National Action Plan to Combat Multidrug-Resistant Tuberculosis,” U.S. Department of Health and Human Services, Washington, D.C., April 1992.
Other books
The Red Door (The Door Series Book 1) by Massey, J. L.
Calder Promise by Janet Dailey
Flirting Under a Full Moon by Ashlyn Chase
Deltora Quest #3: City of the Rats by Emily Rodda
Bound to Please by Lilli Feisty
A Solstice Journey by Felicitas Ivey
Brothers in Blood by Dusty Richards
Red Fortress: History and Illusion in the Kremlin by Merridale, Catherine
It's News to Her by Helen R. Myers
Fevered Hearts by Em Petrova
