Resident Readiness General Surgery (40 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

Alden H. Harken, MD
and Brian C. George, MD
A 65-year-old man arrives, again with a diverticular perforation, but this patient has an old median sternotomy incision and a lump just below his left clavicle. This patient’s BP is 130/90 with a heart rate of 100. By ECG, it looks like the ventricle is being paced, but the atrium is not.
You tell the operating room circulating nurse that you would like to use the electrocautery during surgery. She suggests putting a magnet over the pacemaker.
1.
What triggers a ventricular demand pacemaker to fire?
2.
What does the magnet do?
3.
Is it safe to use electrocautery?
PACEMAKERS AND ELECTROCAUTERY
Answers
1.
The early pacemakers were all “fixed rate” and were programmed to emit one pulse/second, for a ventricular rate of 60. However, occasionally, even patients with complete 3° heart block will exhibit a spontaneous ventricular beat. When the repolarization of this spontaneous QRS (upstroke of the T wave) coincides with a fixed-rate pacer stimulus, ventricular fibrillation may result.
So, the “demand” pacemaker was developed. This type of pacemaker is smart about how it fires. This can more easily be seen with an example. To make the math easier, we will pretend we have a demand pacer with a rate set at 60 beats/min. Every time this “demand” pacemaker senses a QRS complex it turns off and waits for one second. If, at the end of one second, it doesn’t sense another QRS, it fires. So, the patient’s ventricular rate can spontaneously rise above 60, but never below. The trick here is that the pacer can sense many electrical stimuli (like an electrocautery) as a QRS and will stop pacing, but only for as long as you use the cautery. So don’t blast away for long periods.
The ventricular demand pacer prevents the patient from dying; however, it does not increase its rate when the patient runs up stairs. Thus, an atrioventricular pacer coordinates electrodes in both the atrium and the ventricle. When this device “senses” an atrial P wave, it waits a short preset interval (say, 0.18 second), and if it senses a QRS, it turns off; if it doesn’t detect a QRS, it paces one. This device can therefore track faster atrial rates and create atrioventricular
synchrony (adds atrial “kick”). But if the sensed atrial rate ever drops below 60, the A-V pacer paces both the atrium and the ventricle.
2.
Pacemakers are switched into a “fixed-rate” mode whenever a magnet is placed over it. Typically, the fixed ventricular rate is set to 60. If you place a magnet over this man’s pacemaker to convert the pacer into its “fixed-rate” mode, his ventricular rate will actually slow down (from 100 to 60). This would probably be bad for his cardiac output.
3.
Yes, but intelligently. The patient’s demand pacemaker will sense the electrocautery as the patient’s heartbeat and transiently turn itself off. If you use it for too long, that means you’ve stopped the patient’s heart. Therefore, you can use the electrocautery for very short bursts so that the patient will miss only one or two heartbeats during each cauterization. Of course, if you need to use electro-cautery for longer bursts, you can apply a magnet to induce a fixed rate.
TIPS TO REMEMBER
Atrioventricular demand pacing preserves atrioventricular synchrony (ie, the “atrial kick”) as well as tracks faster native atrial rates.
A magnet converts a demand pacemaker to a fixed-rate pacemaker.
Electrocautery effectively suppresses a demand pacemaker’s firing—use it for only as long as the patient can tolerate asystole (typically one or two beats).
COMPREHENSION QUESTIONS
1.
What does the magnet do to a pacemaker?
A. Changes the mode
B. Turns it off
C. Makes it safe to use electrocautery
D. All of the above
2.
What type of pacemaker is most “physiologic?”
A. Fixed ventricular
B. Fixed atrioventricular pacing
C. Demand ventricular
D. Demand atrioventricular pacing
Answers
1.
A
. A magnet changes the pacemaker from a “demand pacing” mode to “fixed pacing” mode. While a magnet does prevent electrocautery from suppressing the pacemaker firing, it is not safer if the fixed rate is too slow to maintain cardiac output.
2.
D
. Look closely at the names of each type of pacing. The “atrio” part of “atrioventricular” means that the pacemaker coordinates ventricular pacing with the atrial beat (via the P wave). That coordination means the ventricular is paced just after the “atrial kick,” which improves cardiac output. It also means that it paces the ventricle faster if the native atrial pacemaker is firing more rapidly. The “demand” part means that the pacemaker kicks in only if the heart doesn’t produce its own beat—again, preserving normal physiologic function whenever possible.
 A Patient With Pulseless Electrical Activity
A Patient With Pulseless Electrical Activity
Alden H. Harken, MD
and Brian C. George, MD
You are in the operating room, in the emergency room, or maybe on the floor. Somebody says “I can’t get a blood pressure.”
You look at the cardiac monitor and there is still electrical activity apparent.
1.
List the 6 H’s and 6 T’s.
2.
Assume that you cannot rule out tension pneumothorax as the cause. Where and how should you decompress it?
3.
Assume that you cannot rule out cardiac tamponade as the cause. What are the landmarks you use to do a pericardiocentesis?
4.
Assume that you cannot rule out hypovolemia as the cause. When would you decide to stop treatment of the patient?
PULSELESS ELECTRICAL ACTIVITY
Answers
1.
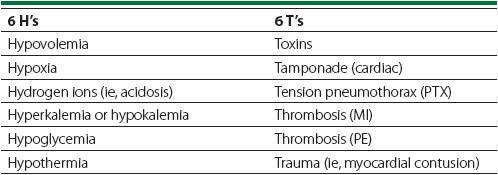
Pulseless electrical activity (PEA) has multiple causes, which you should memorize. During an emergency is not the time to be consulting a reference card (see
Table 32-1
).
Table 32-1.
The Causes of PEA, Organized as the 6 H’s and 6 T’s
Regardless of cause, it doesn’t make any difference whether the patient arrives in the emergency department (ED) with no blood pressure or whether your patient abruptly loses a blood pressure in the operating room—you start with the same “ABC” emergency protocol. You should automatically do the following:
•
Begin bag mask ventilation and start the process of intubating the patient. If the patient is already intubated (eg, in the OR), check the tube.
•
Check the monitor. While pulseless, PEA still implies a cardiac rhythm. If the rhythm strip displays ventricular fibrillation (VF), proceed directly to asynchronous cardioversion (see the Ventricular Tachydysrhythmia Chapter 29).
•
Place 2 large-bore IVs and give some crystalloid.
From this point on, management diverges based on your index of suspicion for each of the possible causes. In general, however, if you cannot rule out a given possibility, then you should empirically treat
before
you’ve made the diagnosis—if you wait to be sure, you’ve waited too long.
Let’s continue the case for some of the more complex yet common scenarios.
2.
In this scenario, let’s assume that your patient is a 70-year-old veteran with a 100-pack/year smoking history. He is undergoing a laparoscopic right colectomy for cancer. At the beginning of the case the anesthesiologist despairs of a peak inspiratory pressure of 45 mm Hg. The cancer is partially obstructing, so you decide to proceed anyway. Midway through the case, the patient loses his pressure. The monitor reveals a heart rate of 130. The tube looks OK. (With an open abdomen, you would feel the aorta in order to confirm hypotension.) You should give 500 mL of LR. Try to listen for breath sounds. Then insert a #18 needle directly up through the diaphragm (if the abdomen is open) or high in the midaxillary (
not
midclavicular) line. You don’t need to connect the needle to anything. Your patient is already on positive pressure ventilation so you cannot produce a pneumothorax. This patient has bought himself a chest tube on the side that produces a gratifying “whoosh” of air.
