Women's Bodies, Women's Wisdom (33 page)
Read Women's Bodies, Women's Wisdom Online
Authors: Christiane Northrup
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #Personal Health, #Professional & Technical, #Medical eBooks, #Specialties, #Obstetrics & Gynecology

Take saunas.
Use a dry brush on skin regularly to help shed old skin and stimulate lymph flow. Brush in the direction of the heart. (These brushes are available at natural food stores.)
 Take a fiber supplement containing both soluble and insoluble fiber, which helps the body excrete excess estrogen and other substances. One of the best such supplements is one to two tablespoons of whole psyllium seed husks in liquid every morning (which are much milder than wheat bran); oat bran or slippery elm is also excellent.
Take a fiber supplement containing both soluble and insoluble fiber, which helps the body excrete excess estrogen and other substances. One of the best such supplements is one to two tablespoons of whole psyllium seed husks in liquid every morning (which are much milder than wheat bran); oat bran or slippery elm is also excellent.
No modern disorder points to the need to rethink our ideas about menstruation and reclaim the wisdom of our cycles more directly than the common malady known as premenstrual syndrome, or PMS. Having treated hundreds of women with PMS, I know that such a rethinking is needed to get to the root causes of PMS. Dietary change, exercise, vitamins, and progesterone therapy are all useful in treating PMS, and I initially recommend them for many women. But in persistent cases of PMS, a deeper imbalance exists that lifestyle changes alone won’t help. As studies have confirmed, unresolved emotional problems may disrupt the menstrual rhythm and the normal hormonal milieu.
57
The reason for this is the intimate connection between our thoughts, emotions, and hypothalamus—the part of the brain that governs the master gland, the pituitary.
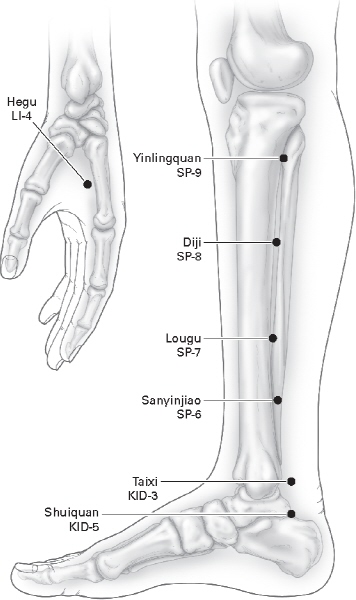
FIGURE 7: ACUPRESSURE POINTS FOR GYNECOLOGICAL PROBLEMS
These are some of the major acupressure points that you can massage to prevent or relieve menstrual cramps. They will often be tender to the touch at first.
Up to 80 percent of all women suffer from PMS.
58
It is most likely to occur in women in their thirties, though it can occur as early as ado lescence and as late as the premenopausal years. PMS has been known since ancient times, but it was popularized in the 1980s by an article in
Family Circle
magazine, which articulated the monthly suffering of millions of women. The media picked up on this, and within a few months PMS became a nationally known problem and a household word.
59
It also became a hot topic with feminists, who argued that the diagnosis would be used against women. Doctors worried that it would become a “wastebasket” diagnosis that women or their families would use as an excuse when no one could figure out what was really going on. Meanwhile, scores of women finally had a name for their monthly suffering and sought medical help for it.
The demand created by women and the media for treatment of PMS had become such that by the mid-1980s, PMS was a lecture topic at many major ob-gyn specialty meetings, and research began ap pearing in the journals. Just as the desire for natural childbirth forced doctors to reform their patriarchal approach to obstetrical practice, women’s desire to understand PMS influenced the practice of medicine and helped move it toward a more enlightened attitude toward the female body.
Diagnosis
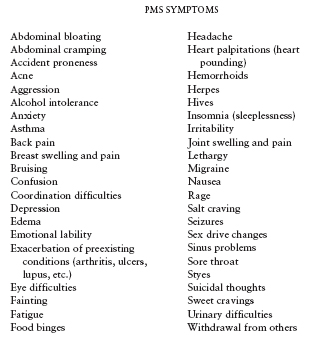
A wide variety of symptoms can be present with PMS. In making the diagnosis, it doesn’t matter what specific symptoms a woman has premenstrually.
What is important is the cyclic fashion in which they occur.
Women who chart their symptoms for three months or more often see a pattern and are able to predict when in their cycle their symptoms are likely to start. Most women will have at least three days during the month when they are entirely free from the symptoms listed here, except in very severe cases. In the second half of the menstrual cycle many underlying conditions are exacerbated, such as glaucoma, arthritis, and depression. Exacerbation of underlying conditions is not defined as PMS, though it is related to PMS. There are more than one hundred known symptoms of PMS.
60
Every one of these symptoms is related to cellular inflammation, resulting from a complex interaction of emo tional, physical, and genetic factors.
If nothing is done to interrupt PMS, it often gets worse over time. In the early stages of PMS, women describe symptoms that arise a few days before their menstrual period and then stop abruptly when the bleeding starts. Then the symptoms gradually begin to appear one to two weeks before the onset of menses. Some women experience a cluster of symptoms at ovulation, followed by a symptom-free week, then a recurrence of the symptoms a week before menses. Over time, a woman may have only two or three days of the month that are symptom-free. Eventually, no discernible pattern of “good” days and “bad” days is left: She feels as if she has PMS virtually all the time.
Some women equate menstrual cramps and PMS, but PMS is different from menstrual cramps (dysmenorrhea). This difference is not always clearly stated in writings on PMS. Many women with PMS have completely pain-free periods. Many women with severe cramping have
no
premenstrual distress. Menstrual cramps are caused by uterine contractions and cramping that results from excess prostaglandin F2 alpha, a hormone produced as the lining of the uterus breaks down during the menstrual cycle. Prostaglandins and other inflammatory chemicals are also involved in PMS symptoms. For that reason, dietary change, vitamin and mineral supplements, and antiprostaglandin medication (usually nonsteroidal anti-inflammatory drugs such as Advil) are often useful both for cramps and for PMS.
61
Though some doctors are still looking for a “biochemical lesion” that causes PMS and hundreds of scientific papers have been published on the topic, no one has been able to find such a lesion or a magic-bullet drug to cure it. A reductionistic approach—looking for the chemical “cause” and “cure”— simply doesn’t work because the causes of PMS are multifactorial and must be approached holistically. The effects of the mind, emotions, diet, light, exercise, relationships, heredity, and childhood traumas must all be taken into account when treating PMS. All combine to create the end result of cellular inflammation, which manifests in many different ways.
All of the following events result in hormonal changes in the body. PMS is apt to be initiated or exacerbated by these changes unless treatment is initiated.
EVENTS ASSOCIATED WITH PMS ONSET
Onset of menses or the year or two before menopause
Coming off birth control pills
After a time of no periods (amenorrhea)
