Welcome to Your Brain (39 page)
Read Welcome to Your Brain Online
Authors: Sam Wang,Sandra Aamodt
Tags: #Neurophysiology-Popular works., #Brain-Popular works

generated at an extremely low rate, so low that some laboratories are unable to detect it at all.
Meanwhile, shrunken cells, dendrites, and axons are capable of growth.
Does the brain recover when a human or animal gives up alcohol? After a few weeks, both brain
volume and function begin to be restored. In animal experiments, cutting off the sauce restores the
dendrites’ complexity. In humans, alcoholics who give up drinking without relapses improve in
cognition and a variety of other abilities, as well as in walking coordination. Human brains even
show evidence of increased volume, which suggests that their brain cells re-expand, as has been seen
in laboratory animals.
Though some of the effects of heavy drinking can be reversed, its consequences can nevertheless
be quite serious. Drinking large quantities of alcohol over a long period of time is associated with
many disorders, including high blood pressure and dementia. Although almost everyone’s brain
shrinks somewhat as they age, the shrinkage that occurs in heavy drinkers seems to be associated with
serious cognitive and neurological deficits.
Furthermore, as we mentioned in
Chapter 1,
years of heavy drinking can lead to a form of
dementia called Korsakoff’s syndrome, in which old memories are lost, and sufferers are unable to
form new memories. In this syndrome, alcoholics develop a thiamine deficiency, which kills neurons
in certain parts of the brain, including the anterior thalamus and mammillary bodies, which are
connected to the hippocampus. These regions are part of the brain’s system for storing new memories
and eventually transferring them to long-term memory. In Korsakoff’s patients, the loss of neurons—
and of function—is irreversible.
A more relevant question for many of us is whether your brain is damaged by moderate
consumption of alcohol. The answer is no. Many people assume that moderate drinking will have the
effects of heavy consumption, only less severe. This is not always the case. Many processes that work
to counteract damaging events can cope better with small events than with large ones. For example,
the blood loss from a small cut is easily recoverable, but severe blood loss may be fatal.
The Japanese study we mentioned earlier showed that ingesting up to fifty grams of ethanol per
day (three to four typical drinks of wine, beer, or liquor) has no measurable effect on brain structure.
The consensus of many studies is that men can have up to three drinks a day, and women up to two
drinks a day without adversely affecting brain structure or cognitive ability (except while you’re
drunk, of course). These numbers are handy because they mean a man and a woman together won’t be
harmed by five drinks, which is the amount of alcohol in a typical bottle of wine. A bottle of Pinot
Noir per day per couple—sounds good to us.
The consumption of red wine may actually be beneficial. Drinking up to three or four glasses per
day reduces the risk of dementia by a factor of two. As little as one glass three or four days a week
can be beneficial, so the range of benign dosages seems to be fairly broad. Unlike hard liquor or beer,
red wine decreases the risk of stroke, say several studies—including one from Bordeaux, France,
where they know a thing or two about red wine.
Dementia can result from the cumulative effect of many small strokes, so it’s likely that by
reducing the risk of stroke, red wine consumption can preserve mental function. What we don’t know
is what is so special about red wine, and whether its alcohol content contributes to the beneficial
effects. If the components of red wine that are responsible for this benefit are ever found, it may be
possible to deliver them without the need to drink wine. This discovery would be useful—though a
bit of a party pooper.
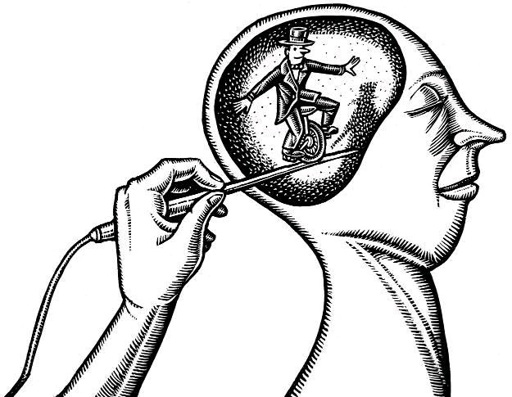
How Deep Is Your Brain? Therapies that Stimulate
the Brain’s Core
Eighteenth-century Italian anatomist Luigi Galvani discovered that the nervous system uses electricity
to convey signals. His assistant noticed that a frog’s legs contracted violently when a nerve was
touched by a metal scalpel. They subsequently found that small electrical sparks delivered to the leg
were sufficient to generate contractions, a discovery that led to the modern understanding that nerves
work by generating electrical impulses. Thanks to his discovery, Galvani’s name has passed into
popular consciousness: when an event suddenly arouses us to awareness or action, we are said to be
galvanized.
Galvani’s discovery eventually gave new hope to sufferers of a variety of neurological disorders,
including Parkinson’s disease and intractable depression. Stimulation deep in the brain’s core can
alleviate symptoms. Patients who receive deep-brain stimulation are galvanized, in the oldest sense
of the word. The treatment can be quite effective, but we have little idea how it works.
Parkinson’s disease strikes adults, usually in their fifties but sometimes earlier. Starting with a
small tremor in voluntary movements, coordination gradually grows worse, and initiating a movement
becomes harder. Late in the disease, patients develop muscular rigidity; even the smallest movements
are slow and require a huge effort. Sufferers shuffle when they walk and often have their faces frozen
in a mask. When Sam met a friend’s wife who has Parkinson’s disease, seconds passed before she
was able to move. In the interim, the only clue to her intention was the focused look in her eyes and an
increasing tremor in her hand, which grew to a marked swing as her desire to shake hands became
apparent.
About 1.5 million people in the U.S. have Parkinson’s disease, which affects about one in one
hundred people over sixty-five. Famous sufferers include actor Michael J. Fox, boxer Muhammad
Ali, Pope John Paul II, evangelist Billy Graham, and former U.S. attorney general Janet Reno. In
some cases, such as Ali’s, a contributing factor was a lifetime of small head injuries. But in general,
the causes of Parkinson’s disease are mostly unknown, as it is not very heritable.
The part of the brain most visibly affected by Parkinson’s disease is the substantia nigra, a region
deep in the brain that appears black in autopsies. The color comes from the neurotransmitter
dopamine, which turns black when it oxidizes. In Parkinson’s patients, these dopamine-producing
cells die.
All treatments for Parkinson’s disease focus on a network of areas in the brain’s core that
coordinate movement. The substantia nigra is just one of a group of neuron clusters, called the basal
ganglia, nestled beneath the cortex. (The basal ganglia, which also include the globus pallidus and the
subthalamic nucleus, communicate with one another and with other brain regions, such as the
striatum.) The first surgical therapy for Parkinson’s disease was to intentionally damage one of the
basal ganglia structures. The idea that damage could be beneficial came from a chance discovery by
neurosurgeons who accidentally ruptured a blood vessel (oops!) that supplies oxygen and glucose to
parts of the thalamus, and found that their mistake had the unanticipated benefit of getting rid of the
patient’s tremor. The surgeons surmised that the death of some part of the affected tissue was
responsible for the relief of the symptoms. This discovery was eventually turned into a strategy in
which a small part of the basal ganglia complex is purposely burned away. This crude treatment,
called a thalamotomy or pallidotomy, is sometimes effective, but did not become widespread since
less than half of patients get any benefit. Even in the patients who do benefit, symptoms return after a
few years.
Another development that made surgery less popular was the advent of a new idea for therapy: if
dopaminergic neurons are dying, why not administer a drug that replaces dopamine? The best drug for
this purpose turned out to be l-dopa, also known as levodopa, a chemical that can enter the brain,
where it gets turned into dopamine. l-dopa and other drugs affecting the dopamine system are now the
most popular therapies for Parkinson’s disease.
Unfortunately, l-dopa only works up to a point. Like all neuromodulators, dopamine has multiple
roles in brain function. For instance, schizophrenia is commonly treated with drugs that block
dopamine receptors. Anti-schizophrenia drugs reduce psychotic delusions but often have the side
effect of inducing muscle rigidity, shuffling gait, and masked facial expressions that look very much
like Parkinson’s disease. Conversely, l-dopa, which acts indiscriminately to strengthen dopamine’s
action everywhere, often leads to psychotic symptoms, such as hallucinations and delusions. As
Parkinson’s disease worsens, the benefit of drug therapy is limited because larger doses are more
likely to trigger psychosis. Worse yet, l-dopa can have mixed positive and negative effects on
movement, causing arms and legs to flail in sudden and unpredictable ways.
l-dopa’s status as the best available therapy changed with a discovery made in 1986 by a French
neurosurgeon who was performing a thalamotomy to correct a persistent tremor. As he worked, he
was able to monitor the patient’s movements and speech because the operation was done without
general anesthesia. (This is possible because surgeons can get through the skin and skull with local
anesthesia, and there are no pain receptors on the inside of the brain.) He used a small probe to
deliver electrical shocks to help him find the place where he should make the lesion. At one location,
he noticed that when he turned up the frequency in the electrode, his patient’s tremor subsided. He
later noted that the improvement he observed during the operation was just as good as the patient’s
performance after the thalamotomy.
This observation suggested that stimulation could somehow lead to an outcome similar to killing a
bit of brain tissue. In the next few years, he tested this idea on patient after patient, giving them
implants and battery packs that they could carry with them, allowing them to receive jolts all day. The
benefits to these patients were striking. Patients who used to need caregivers once again were able to
live independently. Some of them, previously on doses of l-dopa high enough to trigger unacceptable
side effects, now needed far less medication and sometimes none at all. The therapy improved nearly
all types of movement.
In follow-up studies, lasting benefits have been seen for as long as eight years after surgery, as
long as progress has been tracked. The treatment incurs the same risk as all brain surgery: the small
possibility of postoperative bleeding in the brain (see
Chapter 29)
. Although the benefits do decline
with time, perhaps because Parkinson’s disease continues to progress, patients almost always show
long-term improvement. Plus, the new therapy allows patients to avoid the personality changes
brought on by l-dopa treatment. The most common lasting side effect is a gain in weight averaging
nine pounds, which is probably not a deterrent to those who need relief from their disease. By now,
tens of thousands of patients have received stimulator implants. With these successes, it is no wonder
that deep brain stimulation is a preferred treatment for advanced Parkinson’s disease for anyone who
can afford it or whose insurance covers it.
Still, despite the success of deep brain stimulation, we don’t know exactly how it works. First,
it’s odd that stimulating a brain region would produce the same effect as a lesion. Stimulation
probably doesn’t kill brain tissue permanently, since the effects disappear when the treatment is
stopped. One possible explanation is that stimulation has a jamming effect on whatever the
subthalamic nucleus is trying to do. This could happen if stimulation interferes with impulses that
would otherwise be generated in or pass through the subthalamic nucleus. Another possibility is that
the high rate of stimulation reduces the amount of neurotransmitter available for release from
subthalamic neurons, again reducing activity.
A second level of mystery is why blocking a signal from the subthalamic nucleus would help a
parkinsonian brain initiate smooth movements at the right times. One guess is that the subthalamic
nucleus’s normal role is to oppose the substantia nigra’s function. Removing its influence can then
compensate for the loss of nigral function seen in Parkinson’s patients. However stimulation of the
