Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics
Pediatric Primary Care Case Studies (33 page)

Are diagnostics warranted at this point in time?
No red flags were identified to suggest diagnostics are needed. With frequent soiling and a large amount of palpable stool in the abdomen, treatment can begin.
The management of the encopretic child is within the realm of the primary care provider, as long as treatment is approached in a consistent and physiologically oriented way (Levy, 2001). This approach is cost effective and provides faster results than other treatment modalities based on intensive psychological intervention. Once there is improved function, more normal relationships can flourish. For this reason, it is recommended that, unless there are clearly identified psychosocial dysfunction issues, management should concentrate on effective bowel clean-out with subsequent resolution of the soiling. There is time later to refer for mental health intervention if no progress or slow progress is encountered.
Management is based on four key elements (Levy, 2001):

Disimpaction of the rectum and colon:
To stop the soiling and allow normal sensation to return.

Daily stool softening:
To keep the colon clear of stool so it can regain normal tone and the ability to propel stool more effectively.

Establishment of effective toilet habits:
To achieve the goal of evacuating stool at regular times daily.

Parental education:
With the goal of demystification, which allows greater understanding and, hopefully, commitment to treatment.
Disimpaction is necessary before any long-term success can be maintained. It may be accomplished with the use of oral medications or rectal medications. The oral route allows greater sense of control and is less invasive, but compliance can be more problematic. The rectal route is quite invasive and
sometimes traumatic for the child, but is faster and allows the parent more control. The choice of treatment can be determined after discussing options with the child and parents.
When the oral route is selected, high-dose oral electrolyte solutions are recommended (Baker et al., 2006). Although there are no controlled trials demonstrating the effectiveness of high-dose magnesium hydroxide, magnesium citrate, lactulose, sorbital, senna, or bisacodyl for initial disimpaction, these laxatives have been used successfully in that role (Baker et al., 2006).
When the rectal route is preferred, phosphate enemas, saline enemas, or mineral oil enemas followed by a phosphate enema are effective (Baker et al., 2006).
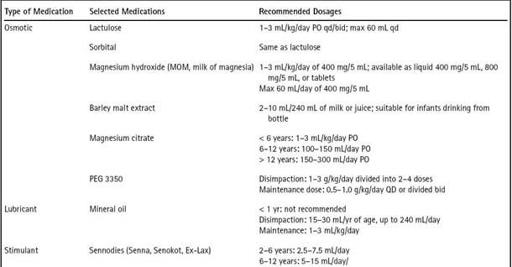
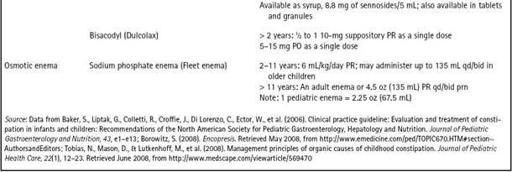
Disimpaction is typically completed using oral medications. Dosages of various medications used in treatment of constipation/impaction are found in
Table 9-3
. Most disimpactions can be completed at home. On occasion, children may have to be admitted to the hospital for disimpaction. A nasogastric tube is placed, and PEG 3350 (Miralax) with electrolytes is administered until rectal effluent is clear.
Following discussion with Zachary and his parents, it was decided to use an over-the-counter electrolyte solution, PEG 3350. Because it has no taste or texture and dissolves readily in fluids, it is easy to administer. Magnesium citrate is quite effective and typically promotes a faster clean-out, but it is quite sour tasting and is difficult for many children to accept. PEG 3350 also tends to have less association with abdominal cramping than magnesium citrate.
Zachary’s parents were instructed to mix 17 g of PEG 3350, which is measured easily by the bottle’s cap, with 8 ounces of a beverage of choice, which gives about 2 g PEG 3350 per ounce. Beverages can be cold or hot, clear or milk products, and the beverage with PEG mixture is good in the refrigerator for 48 hours. PEG 3350 is not to be mixed with foods. The recommended clean-out dose of PEG 3350 is 1.5 g/kg/day. Zachary weighs 65 pounds (30 kg), so he needs 44 g of PEG 3350 per day in divided doses, which is approximately 22 ounces per day of the PEG 3350/fluid mixture. He is to drink this dose of PEG 3350 daily until his stool is very runny. The amount of time needed to complete a bowel clean-out is quite variable, but commonly takes 4–5 days.
Initially, stool may be quite loose as the softer leakage is cleaned out first. The hard stool then begins to break down and stool will be quite grainy and thick for a number of days, before it finally starts to thin and become a “thin mud puddle.” An effective clean-out has not occurred until you reach this point. Because Zachary is in school, his parents have been instructed to begin the clean-out over the weekend and anticipate missed days of school. Teachers should be advised of his absence and have work sent home. To promote faster evacuation of stool, a stimulant, bisacodyl, can be added to the daily regimen giving one 5 mg tablet orally once or twice a day. During the clean-out, many children feel nauseated and have stomachaches and/or emesis; however, the clean-out should not be stopped unless symptoms are severe.
Table 9–3 Medication for Use in Treatment of Encopresis/Constipation
Once a bowel clean-out is completed and Zachary is having watery stools, stimulant medication is discontinued and the PEG 3350 dose is decreased to half the initial clean-out dose. Zachary’s maintenance phase begins with the decreased dose. The maintenance dose of PEG 3350 is about 8 g/kg/day in a single dose or divided. Zachary is instructed to return to the office in 3 weeks and call as needed for assistance.
Maintenance or Daily Stool Softening
Once the impaction has been removed, the treatment focuses on the prevention of another impaction. At this point, soiling should significantly decrease or resolve. It is important to have full evacuation of stool from the colon and that stools be soft and easy to pass, be nonpainful, and be difficult to withhold. This is especially paramount for the toddler with active stool withholding related to pain with defecation. There is no correct dose of daily stool softener, but rather enough daily medicine should be given to produce one to three soft, mushy, milkshake-consistency stools. During the first month of maintenance, a stooling calendar charting all stools and their consistency should be logged.
Dietary changes are commonly advised. Recommendations have focused on increasing fluids and fiber in the diet to promote passage of stool; however, the literature is mixed on this issue. A balanced diet that includes whole grains, fruits, and vegetables is recommended as part of the treatment for constipation in children (Baker et al., 2006; Levy, 2001). Milk and cheese should be eaten sparingly because they can cause constipation. Forceful implementation of a high fiber diet is undesirable and often not worth the power struggle it invites.
Next Visit
Zachary is seen back at the office following a bowel clean-out that took 5 days to reach “dirty water” bowel movements. Bisacodyl is discontinued, and he continues to take 12 ounces of the PEG 3350 mixture daily. He is having two soft, milkshake-consistency stools in the toilet every day and soiling has stopped. Zachary finally smiles as he talks to you. Urinary incontinence has resolved. On exam, his abdomen is soft, nontender, and without palpable fecal mass. Zachary and his parents are pleased.


