Pediatric Primary Care Case Studies (30 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

Breastfeeding Observation
Prior to observing a feeding, you examine Mrs. Jackson’s breasts. Her breasts are slightly firm with nipples that appear somewhat flat but evert with tactile stimulation. There are no cracks or bleeding visible. You are able to hand express drops of milk from both breasts.
Observation of a breastfeeding session reveals that Peter latches on successfully but starts to get drowsy fairly quickly. Positioning is adequate in the “cradle” position but Mrs. Jackson is reminded to keep him “tummy to tummy” as Peter falls away from the breast as he goes to sleep. Mr. Jackson attempts to help by talking to Peter and stroking his back. Meanwhile, Mrs. Jackson makes a few attempts to wake him but then gives up and shrugs her shoulders as if to say that this is typical. When removed from the breast and stimulated with a cold wet washcloth on his trunk, Peter wakes up again. Regular stimulation with gentle but persistent scratching to the soles of his feet and top of his head helps him stay with feeding. Periodically Peter is taken off, given additional stimulation, and switched to the other side if he does not respond to wakening techniques at the breast. He ends up at the breast for more than 30 minutes—most of which is alert feeding. He has gone back and forth twice to each breast. Some loud swallows are heard briefly at the beginning on each side. After feeding, he weighs 6 pounds 8.5 ounces on the same scale he was weighed on prior to your seeing him, a gain of 1.5 oz. Mom and dad are somewhat relieved by this news.
Making the Diagnosis
Given the histories of the mother and baby as well as the feeding history, the physical examination, and breastfeeding assessment/observation, the problem appears to be slow weight gain.
In assessing slow weight gain, a helpful way to approach the evaluation is to identify risk factors that are mother-related, infant-related, and/or technique-related (Lawrence & Lawrence, 2005). In this case, the mother has no chronic illness, takes no medications routinely, and her vaginal bleeding has stopped. Her breast exam reveals no significant issues as her nipples evert with stimulation, there are no cracks or bleeding, she is not engorged, and breastmilk is expressible from both breasts. There are no red flags for maternal health issues other than that she is a first-time mother and seems unclear about expected feeding frequency and output. She is producing milk for her baby.
The baby is afebrile and not visibly jaundiced. Key information obtained includes the following:
• Special attention should be paid to evaluation of the heart to rule out congenital heart disease that may not have been apparent before hospital discharge. There is no murmur and his pulses are normal.
• The suck is strong, and the palate is intact. Submucosal clefts can result in poor weight gain and need to be ruled out.
• This baby has no evidence of positive physical findings related to infection, hyperbilirubinemia, or dehydration.
• However, this baby was born at 37 weeks and should be considered a “late preterm infant.” Sleepiness and slow feeding are common in the slightly preterm infant, despite a healthy birth weight and absence of other problems associated with prematurity (Meier, Furman, & Degenhardt, 2007).
The technique issues are primarily related to feeding frequency and duration, although inefficient suckling with inadequate milk transfer must also be considered. Mrs. Jackson is using proper positioning and gets latch-on with little difficulty. Peter gained 1.5 ounces after an alert and persistent feeding. That is very good news, and seems to confirm that his lack of weight gain is likely not related to health problems for him or his mother.
Successful breastmilk production is based on supply and demand. Regular, frequent stimulation with a successful latch, routine emptying of the breast, and the release of maternal hormones aid in the establishment of an adequate milk supply to sustain infant growth (Hellings, 2009). Peter has not been feeding the expected 10–12 times in 24 hours, and quality feedings have been of short duration.
After consideration of the possibilities, the most likely expanded diagnosis is slow weight gain due to inadequate feeding frequency and duration.
Management
The Jacksons are sent home with instructions to feed Peter every 2–3 hours for the next 24 hours and to use the awakening techniques demonstrated. They are reminded to set an alarm if necessary to wake themselves and to count the interval between feedings as the time from the start of one feeding to the start of the next. They are asked to keep a diary of feedings—time feeding started, duration, and a statement about quality of the feed—and number of voids and stools. Finally, they are asked to return tomorrow to check on progress. Mr. and Mrs. Jackson indicate that they think this is something they can do for 24 hours and they both state they really want the baby to be breastfed.
Important Considerations in Making the Management Plan
It is good that the parents came in so soon and that the mother’s supply does not appear to have markedly decreased at this time. The weight gain associated with the feeding in the clinic also provides support for sending the family home with clear instructions regarding feeding. Supplementation is not necessary at this time; however, early follow-up to make sure that Peter continues to gain weight is very important.
Follow-Up Visit #1
The Jacksons return the next afternoon. They look tired and state they did not get much sleep last night. However, they think Peter has been doing better with feedings. In reviewing their diary, you note the feeding frequency and duration, wet diaper counts, and stool output. They still have to stimulate him a bit, but he has fed nine times in the last 24 hours. He had
one large, loose, curdy, slightly greenish stool at 5 a.m. You commend them for their efforts. Mrs. Jackson does state that her nipples are sorer than yesterday. They are anxiously awaiting his weight check to see if their feeding efforts have been successful.
Important considerations in the follow-up examination:
Peter’s general appearance is important to note. In addition, he should be weighed on the same scale as yesterday. A full physical examination was completed yesterday and need not be repeated today.
Physical Examinations of Infant and Mother
Peter is alert and responsive. His cheeks look fuller. He weighs 6 pounds 9 ounces, an overall gain of 2 ounces in 24 hours. Mrs. Jackson says that her breasts feel fuller between feedings.
As Mrs. Jackson prepares to feed Peter, you examine her breasts again. You note some redness and a chapped appearance on the nipples. There is no cracking or bleeding. You review positioning and latch-on techniques with her as she puts Peter to breast. She states that she can feel the difference between a good latch and a poor one as you take him on and off several times to secure a good latch. You advise her to reposition him if the latch is painful rather than trying to ignore the pain. She finishes feeding Peter before they return home with another scheduled weight-check appointment in 2 days and instructions to call with any questions.
Peter has gained 2 ounces in 24 hours and has stooled once. The frequent feedings with poor technique at times has resulted in some increased nipple tenderness and irritation for Mrs. Jackson. With better technique and continued attention to feeding frequency and duration, the parents can go home and continue with the plan.
Follow-Up Visit #2
Mrs. Jackson is smiling and feeling confident that he has gained more weight. She states that her husband had to return to work so she came alone this time with Peter. He is 11 days old and is waking up now on his own to feed and fed 10 times in the last 24 hours. He stooled three times in the last 24 hours and the most recent one was runny, yellow-orange in color, and very curdy. She states that her nipples are less sore and admits that she did not set the alarm last night. Peter awakened on his own every 2 to 2.5 hours, with one stretch of 3 hours during the night.
Physical Examinations of Infant and Mother
Mrs. Jackson’s nipples no longer have a chapped appearance but are still a little red. The skin remains intact. Her breasts are full, and she begins to actively leak milk during her exam. She puts Peter to breast with no difficulty, and he begins to feed vigorously with audible swallows.
Peter is awake and alert during the feeding. He requires no stimulation to keep feeding. He weighs 6 pounds 14 ounces, 1 ounce above birth weight and 5 ounces more than 2 days ago.
Because he is feeding well, you go ahead and get the second metabolic screening test done. Mrs. Jackson is really happy and gets out her cell phone to call her husband and share the news.
Peter gained 5 ounces in 2 days, more than the ½ to 1 ounce per day gain usually expected. He has been gaining at a “catch-up” rate. He is likely to continue at this rate for only a few more days and will then slow down to the normal expected daily weight gain. He has reached birth weight, an important milestone. Peter should return in 1 week to make sure he continues to gain weight. The parents should be encouraged to call with questions and are provided with information about how to assess if he is getting enough breastmilk.
What problems were avoided by this quick intervention and what could have been done preventively to avoid this breastfeeding problem?
This case study details a common clinical scenario in pediatric primary care. This time, there is a happy ending with a baby gaining weight on exclusive breastfeeding and with more confident parents. The story might have played out differently if the parents had delayed seeking assistance or if the mother’s milk supply had been more compromised.
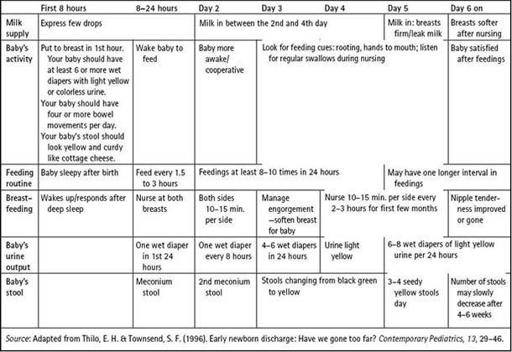
The problems might have been avoided if early assessment at the 3-day postdischarge visit had taken place and the slow feeding identified and managed. It is imperative to emphasize to parents the importance of that early follow-up visit, especially for the breastfeeding family. In addition, providing verbal and written information regarding expectations for breastfeeding and urine/stool output at the time of discharge from the hospital can be very helpful to parents, especially first-time parents, as they begin to care for their newborns (see
Table 8-6
).
In the assessment process for each individual patient, other problems might be found that suggest more complex health concerns for mother or baby. The need to carefully consider potential risk factors for insufficient infant weight gain is an important part of an initial breastfeeding visit.
Key Points from the Case
1. Early follow-up of breastfeeding families and assessment/identification of problems are important for supporting successful breastfeeding.
2. Common breastfeeding problems do not always require the services of a lactation consultant. However, primary care providers need to have a knowledgeable approach to the assessment and management process.
3. The assessment process includes recognition and identification of problems in the baby, mother, and breastfeeding technique.
4. Management strategies for slow weight gain must take into account issues for the baby, the mother, and breastfeeding technique.
Table 8–6 Guidelines for Breastfeeding in the First Few Days
REFERENCES
American Academy of Pediatrics. (2005). Breastfeeding and the use of human milk.
Pediatrics, 115
, 496–506.
Healthy People 2010. (2000).
National health promotion and disease prevention objectives
. DHHS Pub. No. 91-50213. Washington, DC: Government Printing Office.

