Pediatric Examination and Board Review (65 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(A) nutritional rickets
(B) hypoparathyroidism
(C) X-linked hypophosphatemic rickets
(D) PHP
(E) PPHP
6.
In nutritional rickets, which of the following laboratory values would you expect to be low?
(A) parathyroid hormone (PTH)
(B) 1,25-dihydroxyvitamin D
(C) 25-hydroxyvitamin D
(D) alkaline phosphatase
(E) B and C
7.
The radiograph shown in
Figure 41-1
is most representative of which of the following?
(A) hypoparathyroidism
(B) PHP
(C) nutritional rickets
(D) PPHP
(E) hyperparathyroidism
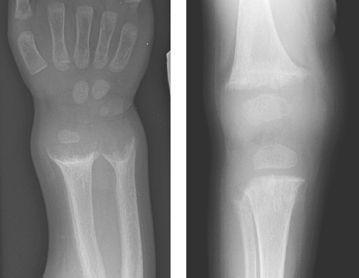
FIGURE 41-1.
Radiograph of the wrist (left) and knee (right) in a 14-month-old child with a seizure.
8.
Rachitic bone deformities include which of the following?
(A) craniotabes
(B) rachitic rosary
(C) Harrison grooves
(D) A and B
(E) all of the above
9.
You start the child on intravenous (IV) calcium replacement, but the serum calcium does not normalize. Which of the following should you look for?
(A) hypokalemia
(B) hypoglycemia
(C) hypomagnesemia
(D) hypophosphatasia
(E) hypophosphatemia
10.
PTH controls serum calcium levels through its action on all of the following organs except which of the following?
(A) bone
(B) kidney
(C) liver
(D) intestinal tract
(E) C and D
11.
The active form of vitamin D is which of the following?
(A) 25-hydroxyvitamin D
(B) 24,25-dihydroxyvitamin D
(C) vitamin D
2
(D) vitamin D
3
(E) 1,25-dihydroxyvitamin D
12.
The major impact of the active form of vitamin D is on which organ?
(A) parathyroid glands
(B) kidney
(C) intestinal tract
(D) bone
(E) liver
13.
Which of the following is not a typical cause of early neonatal hypocalcemia (within the first 72 hours of life)?
(A) prematurity
(B) infant of a diabetic mother
(C) congenital hypoparathyroidism
(D) asphyxia
(E) small for gestational age
14.
Late neonatal hypocalcemia (between 5 and 10 days of life) is most likely caused by each of the following except
(A) asphyxia
(B) transient hypoparathyroidism
(C) hyperphosphatemia
(D) infant of a mother with marginal vitamin D intake
(E) hypomagnesemia
15.
You diagnose your patient with nutritional rickets because of vitamin D deficiency. You would likely use all of the following except which in your management of the patient?
(A) calcium supplementation
(B) phosphate supplementation
(C) calcitriol (1,25-dihydroxy vitamin D)
(D) ergocalciferol (vitamin D
2
)
(E) B and D
16.
Your patient has a low calcium, low phosphate, and elevated alkaline phosphatase. You acutely start the child on IV calcium, calcitriol (1,25-dihydroxyvitamin D), and oral ergocalciferol. The calcium normalizes quickly with your therapy. After several days, you stop the calcitriol, and to your surprise, the calcium level falls. What is the most likely cause?
(A) laboratory error
(B) development of hyperphosphatemia
(C) patient remains hypophosphatemic
(D) the patient received too much calcium
(E) patient has 1-α-hydroxylase deficiency
17.
You diagnose your patient with hypoparathyroidism, and once the serum calcium is stabilized, you discharge him home on calcitriol and supplemental calcium. The mother calls in 1 week complaining that she is changing her child’s urine-soaked diaper every 2 hours. What should you be most concerned about?
(A) hypermagnesemia
(B) hypomagnesemia
(C) hypocalcemia
(D) hypercalcemia
(E) hyperphosphatemia
18.
What test(s) would help in the diagnosis if your patient was an infant with hypocalcemia and cardiac defects?
(A) chest radiograph
(B) analysis of chromosome 15q11
(C) analysis of chromosome 22q11
(D) A and B
(E) A and C
ANSWERS
1.
(C)
Hypocalcemia. Chvostek sign is a twitching of the circumoral muscles in response to gentle tapping on the facial nerve just anterior to the ear. It is a sign of hypocalcemia; however, up to 10% of normal individuals have a slight twitch in response to this maneuver.
2.
(B)
Laryngospasm, prolonged QT interval on ECG, and a positive Trousseau sign. The signs and symptoms of acute hypocalcemia typically result from increased neuromuscular irritability. This can be elicited by checking for a positive Chvostek or Trousseau sign. Trousseau sign is carpal spasm seen with hypoxia. To test for Trousseau sign, a blood pressure cuff should be inflated to 20 mm Hg above the patient’s systolic blood pressure for 3 minutes.
Figure 41-2
shows the classic response of a positive Trousseau sign. Unlike Chvostek sign, which can be seen in patients with normal calcium levels, a positive Trousseau sign is rare in the absence of hypocalcemia. Patients often complain of paresthesias of the fingers, toes, and circumoral region. Muscle cramps are also seen and may progress to tetany (spontaneous carpopedal spasm). Laryngospasm and bronchospasm can be seen. Other signs and symptoms include seizures, irritability, impaired school performance, and behavioral changes. With severe hypocalcemia, patients can have prolongation of their QT interval and can be prone to arrhythmias.
3.
(A)
Nutritional rickets. Children with nutritional rickets usually present with both low serum calcium and phosphate because of a deficiency of vitamin D, leading to a decrease of both calcium and phosphate absorption in the gut. Rickets can also develop with a deficiency of either calcium or phosphate, especially in the rapidly growing premature infant. Hypoparathyroidism and PHP usually present with hyperphosphatemia because of a lack of PTH action on the kidney where PTH typically stimulates excretion of phosphate. Children with PPHP have the phenotypic features of Albright hereditary osteodystrophy (PHP type 1a) without the biochemical abnormalities. X-linked hypophosphatemic rickets occurs because of a defect in the kidney causing a loss of phosphate, but these children do not present with hypocalcemia.
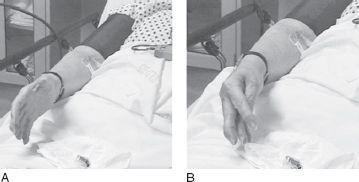
FIGURE 41-2.
An example of the Trousseau sign. The photo on the right demonstrates flexion of the wrist and metacarpophalangeal joints, with extension of the interphalangeal joints and adduction of the finger after insufflation of the blood pressure cuff. (Reprinted with permission from Meininger ME, Kendler JS. Trousseau’s sign.
N Engl J Med.
2000;343:1855. Copyright 2000 Massachusetts Medical Society. All rights reserved.)
4.
(B)
Hypoparathyroidism. Hypoparathyroidism occurs when the PTH produced by the parathyroid glands is insufficient to maintain the serum calcium in the normal range. Because PTH causes renal calcium absorption and renal phosphate excretion, insufficient PTH causes both hypocalcemia and hyperphosphatemia. Serum PTH is low, serum 1,25-dihydroxyvitamin D is usually low to low normal (PTH enhances the conversion of 25-hydroxy- to 1,25-dihydroxyvitamin D), and alkaline phosphatase is usually normal.
5.
(D)
PHP, which is a syndrome characterized by target tissue unresponsiveness to the actions of PTH. Biochemical abnormalities of hypoparathyroidism are seen including hypocalcemia and hyperphosphatemia in the face of elevated PTH levels. PHP type 1a is also called Albright hereditary osteodystrophy, which presents with PTH resistance with other somatic defects including short stature, round facies, obesity, and developmental delay.
6.
(C)
25-Hydroxyvitamin D. In nutritional rickets, hypocalcemia causes a secondary hyperparathyroidism, and thus PTH levels will be elevated. Because PTH and hypophosphatemia stimulate renal production of 1,25-dihydroxyvitamin D, levels of this hormone will be normal to high. Alkaline phosphatase is a marker of bone turnover that tends to be elevated in nutritional rickets. 25-Hydroxyvitamin D reflects the nutritional component of vitamin D, and these levels would be low in vitamin D–deficient rickets.
7.
(C)
Nutritional rickets. The radiograph demonstrates typical findings of nutritional rickets including widening with cupping and fraying of the metaphyses. The bones are often demineralized in general. In general, no bone changes are seen in hypoparathyroidism and PHP. Occasionally, bone changes consistent with hyperparathyroidism such as subperiosteal and endosteal bone resorption can be seen in PHP because of the bones not being resistant to PTH.
