Pediatric Examination and Board Review (36 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

On examination, the child is thin, notably picking and scratching at her arms and legs. She is quiet and withdrawn. There are widespread ill-defined plaques of dry, excoriated, and thickened skin with scale over the extremities predominantly, with less thickened patches on the trunk. There are areas of fissuring and erosion, and crusty exudates, particularly on the legs and near the elbows. In the folds of the elbow and knee, there are deeper erosions revealing red raw skin, also some clustered vesicles (see
Figure 19-1
). There is widespread lymphadenopathy.

FIGURE 19-1.
See color plates.
SELECT THE ONE BEST ANSWER
1.
Appropriate care of this patient will include
(A) administration of oral corticosteroids
(B) application of topical antibacterials
(C) application of topical antihistamines
(D) administration of oral antibiotics
(E) limitation of bathing to once weekly with a 30-minute soak
2.
The finding of clustered vesicles also raises concern for
(A) chickenpox infection
(B) sexual abuse
(C) allergic contact dermatitis
(D) hand, foot, and mouth disease
(E) eczema herpeticum
3.
The most helpful diagnostic test to evaluate the vesicle would be
(A) patch testing
(B) bacterial culture
(C) viral culture
(D) direct fluorescent antibody testing
(E) scraping and staining with KOH
4.
Initial topical therapy for this patient should include
(A) mid-potency topical corticosteroid ointment under wet wraps
(B) topical antihistamine cream
(C) topical calcineurin inhibitor cream
(D) high-potency topical corticosteroid cream
(E) wet to dry dressings
5.
Skin care recommendations in this setting should include
(A) regular long hot soaks in a bathtub
(B) daily short baths in tepid water
(C) regular use of antibacterial soaps
(D) avoidance of topical lubricants
(E) limitation of bathing to once weekly with a 30-minute soak
6.
The least well-established trigger of flares of this nature is
(A) secondhand cigarette smoke
(B) dust
(C) milk protein
(D) animal dander
(E) fragrance
7.
This patient’s 8-year-old brother is also complaining of an itchy rash on his belly and arms that has been present for months. On examination, you notice an ill-defined plaque of excoriated and hyperpigmented papules infraumbilically (
Figure 19-2
A) and fleshcolored papules over his extensor arms and legs (
Figure 19-2
B). You recommend that he
(A) keep his shirt tucked in at all times
(B) avoid skin contact with the metal button on his jeans and his belt buckle
(C) follow the same skin care recommendations you gave his sister
(D) be treated for scabies
(E) take griseofulvin by mouth for 2 months
8.
The most common contact allergen in the United States is
(A) laundry detergent
(B) fragrance mix
(C) nickel
(D) neomycin
(E) peanut
9.
A 5-year-old girl presents to your office with a 1-week history of red scaly 1- to 3-cm plaques predominantly over her trunk and extremities. She states she has otherwise been feeling well, but her mother notes a bit more fatigue than usual. You note that the patient is afebrile, but her tongue and oropharynx are erythematous and the rash is randomly distributed on the trunk (
Figure 19-3
). You immediately suspect a diagnosis of
(A) pityriasis rosea
(B) guttate psoriasis
(C) scarlet fever
(D) mononucleosis
(E) toxic shock syndrome
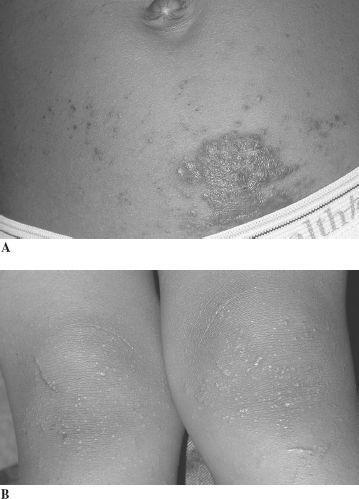
FIGURE 19-2.
See color plates.
10.
The best test to do is
(A) a throat culture
(B) a monospot test
(C) a skin biopsy
(D) scraping and staining with potassium hydroxide
(E) an antinuclear antibody (ANA)

FIGURE 19-3.
See color plates.
11.
You tell the family to expect
(A) the rash will resolve in a week followed by widespread desquamation
(B) the rash will resolve in 6-8 weeks with postinflammatory dyspigmentation
(C) the rash will improve with treatment but may persist to some degree for life
(D) the patient will have to discontinue all contact sports
(E) sun protection is paramount
12.
A 9-month-old infant presents with a worsening rash in the preceding month. Her mother states that the child is quite irritable and is having looser stools. She has been applying hydrocortisone with minimal improvement. On examination, there are erythematous scaling and eroded plaques on the cheeks and around the mouth, also on the lower abdomen, in the diaper area, and over the hands and feet. A helpful piece of history concerns
(A) whether there has been any change in diet
(B) whether there are new pets in the household
(C) whether there are any sick contacts
(D) whether the child is in day care
(E) whether the family is using a new laundry detergent
ANSWERS
1.
(D)
The patient described is presenting with an acute flare of severe atopic dermatitis. The finding of crusting exudates and erosions is strongly suggestive of secondary bacterial infection. Additionally it is known that patients with chronic atopic dermatitis are frequently colonized by bacteria such as
S aureus
, and it is thought that the presence of the organism may drive the inflammatory reaction in the skin. Systemically administered antibiotics are much more effective for decreasing the overall carriage rate of the bacteria and treating the secondary infection. Systemic corticosteroids are rarely indicated in the management of atopic dermatitis and should not be considered first-line treatment. Topical antihistamines are often sensitizing, leading to allergic contact dermatitis, especially in patients with a defective skin barrier; therefore, topical agents are not recommended in this setting. Additionally, systemic absorption of these agents when applied to large surface areas in young children, especially those with a compromised skin barrier, can lead to toxic levels. Bathing recommendations are controversial, but daily short baths with appropriate skin care following can be therapeutic.
2.
(E)
Eczema herpeticum refers to a generalized eruption of herpes simplex virus infection in a patient with a compromised skin barrier, such as during a flare of atopic dermatitis. A history of cold sores within the family may be suggestive. The finding of clustered round punched-out erosions and vesicles in the setting of atopic dermatitis is also suggestive of this potentially severe secondary infection. It is uncommon to see an active case of chickenpox in this setting. An acute allergic contact dermatitis can be exuberant and present with vesicles but typically will affect a limited surface area with relatively well-demarcated borders or follow geographic patterns, such as the linear streaks from poison ivy. Hand, foot, and mouth disease typically is associated with small shallow erosions on the hands, feet, and oropharynx. Sexual abuse is not the primary concern in this setting as the acquisition of HSV is extraordinarily prevalent.
3.
(D)
The direct fluorescent antibody tests for herpes viruses can be accomplished very quickly and provide guidance for treatment of possible cases of eczema herpeticum. The most reliable specimen is taken from the base of an intact vesicle. The vesicle should be gently unroofed, and the base then rubbed with a cotton applicator and transferred to a microscope slide. Patch testing is done to determine sensitivity to contact allergens. Bacterial and viral cultures may also be helpful in this setting but will not provide as rapid results. Potassium hydroxide preps are useful to confirm suspected tinea infections.
4.
(A)
Appropriate care of a patient with a widespread flare of atopic dermatitis involves very specific instructions to the family regarding skin care. The mainstay of therapy will be the use of a topical corticosteroid preparation. These agents have a long history of safety and efficacy in this setting. Choice of an appropriate-strength agent is critical. The age of the patient, extent of surface area to be covered, and sites of application will all help determine the most appropriate potency. High-potency agents are only rarely used in children, and when used are most often used only on hands or feet and for very limited periods of time. Mid-potency agents used under occlusion with warm wet linens accomplishes hydration as well as healing. Ointment-based products provide more occlusive and emollient effects than creams and lotions, and thus they are more effective in the setting of acute flares. Topical antihistamines, as mentioned previously, may cause sensitization. The newest agents in the armamentarium against atopic dermatitis are the topical calcineurin inhibitors. These agents are anti-inflammatory in the skin and seem to cause minimal systemic absorption. They do not cause cutaneous atrophy. However, they may not be as effective as topical steroids in the setting of an acute flare. Additionally, the risks of long-term use are still unknown. Wet to dry dressings do not have a role in this setting.
