Pediatric Examination and Board Review (13 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(E) 220 mg/100 mL
10.
Which of the following is not a common cause of secondary hypercholesteremia in children?
(A) obesity
(B) isotretinoin
(C) oral contraceptive pills
(D) hyperthyroidism
(E) anorexia
11.
What is the most common form of inherited hyperlipidemia?
(A) familial hypercholesterolemia
(B) familial combined hyperlipidemia
(C) mild hypertriglyceridemia
(D) severe hypertriglyceridemia
(E) none of the above
12.
Which of the following is a true statement regarding the treatment for hypercholesterolemia in children?
(A) a Step 1 diet is recommended for children younger than 2 years of age
(B) bile acid sequestrants are recommended for children older than 10 years of age when diet modification alone is not effective
(C) lovastatin may be used in selected cases for children younger than 2 years of age
(D) none of the above
(E) all of the above
13.
A 10-year-old child with physical features of tall stature, a long thin face, scoliosis, pectus excavatum with a family history of sudden death at a young age (an uncle who died while playing basketball) presents for a preparticipation sports physical. What is the likely diagnosis in this patient?
(A) Marfan syndrome
(B) hypertrophic cardiomyopathy
(C) Turner syndrome
(D) Down syndrome
(E) homocystinuria
14.
What is the most common cardiac lesion associated with this 10-year-old’s diagnosis?
(A) mitral valve prolapse
(B) aortic stenosis
(C) coarctation of the aorta
(D) left ventricular outflow tract obstruction
(E) atrial septal defect
15.
An echocardiogram is ordered and demonstrates mild aortic root dilation. What is the recommendation for further management?
(A) participation in sports is unrestricted
(B) follow-up echocardiogram in 10 years
(C) return to clinic only if symptoms of chest pain occur during activities
(D) treatment with beta-blockers may decrease the risk of further aortic root dilatation
(E) aortic root replacement
16.
What findings during routine pre-participation physical examination would place a child at risk for sudden death during sports?
(A) a harsh systolic murmur at the upper right sternal border
(B) family history of diabetes
(C) respiratory sinus arrhythmia
(D) a single elevated blood pressure reading that returns to normal on subsequent visits
(E) arm span less than height
ANSWERS
1.
(B)
Hypertension is defined as a systolic or diastolic blood pressure recording greater than the 95th percentile for age and gender, recorded on 3 separate occasions. Severe hypertension is defined as blood pressure recordings greater than the 95th percentile by 8-10 mm Hg. Accurate blood pressure recordings are crucial for this diagnosis and should be taken in a quiet, nonthreatening manner. The width of the blood pressure cuff should be 40-50% or more of the arm circumference. Smaller blood pressure cuffs result in erroneously high blood pressure recordings. Ideally, blood pressure recordings should be taken in all 4 extremities. Anxiety leading to transient elevations in blood pressure (white coat hypertension) accounts for up to 40% of elevated blood pressure recordings in children. Because the diagnosis of hypertension should not be based on a single reading, medical therapy and testing for secondary causes of hypertension are not appropriate during this first visit.
2.
(A)
Hypertension is classified as either primary (essential or idiopathic) or secondary. Primary hypertension is the most common syndrome in older patients such as this child, whereas secondary hypertension is common in younger patients with more severely elevated blood pressure recordings. Ninety percent of secondary causes are because of renal parenchymal disease, renal artery disease, and coarctation of the aorta.
3.
(D)
Renal parenchymal hypertension causes salt and water retention and in some cases elevated renin levels leading to increased vascular resistance. Increased serum catecholamine levels causing hypertension are seen with pheochromocytomas or with congenital adrenal hyperplasia (11-hydroxylase deficiency or 17-hydroxylase deficiency). Hypertension is also seen with use of certain drugs or medications and in cases of hypercalcemia.
4.
(A)
The initial evaluation of hypertension is guided by both the examination and the family history. The important features of the history include a past medical history of urinary tract infections, cardiovascular surgeries, weakness or cramps, medication use, and tobacco use. Important features of the family history include history of hypertension or premature heart disease. The important features of the physical examination include accurate blood pressure recordings in 4 extremities, assessment for heart murmurs or bruits, assessment of peripheral pulses, assessment of renal tenderness, and a thorough eye examination. The usual initial laboratory evaluation includes a urinalysis, serum electrolytes including blood urea nitrogen (BUN) and creatinine, and possibly a 12-lead ECG, chest radiograph, and echocardiogram. A cholesterol level and a lipoprotein analysis are indicated in select cases. If there is severe hypertension and end-organ involvement or hypertension refractory to therapy, then tests evaluating for secondary causes of hypertension can be performed.
5.
(A)
Additional management in patients with hypertension includes nonpharmacologic interventions such as exercise proscription, weight reduction, avoidance of tobacco or oral contraceptive pills, and reduction of dietary salt intake. In severe hypertension or persistent hypertension despite nonpharmacologic interventions, pharmacologic agents are often used that include diuretics, beta-blockers, and vasodilators.
6.
(C)
Beta-blockers are often used in conjunction with diuretics or in conditions where hyperthyroidism results in hypertension. However, they are contraindicated for use in patients with asthma (can precipitate bronchospasm), diabetes (prevents manifestation of symptoms of hyperglycemia), and in patients with bradycardia.
7.
(A)
A hypertensive emergency requires immediate reduction of blood pressure usually within minutes to hours. Hypertensive crises can be associated with neurologic signs or congestive heart failure. Administration of parental medications is important for the acute treatment of hypertensive emergencies. These medications include diazoxide, nitroprusside sodium, diuretics, IV nifedipine, hydralazine, or labetalol. Phentolamine is usually reserved for patients with pheochromocytomas.
8.
(A)
Hypercholesterolemia is a major risk factor for coronary artery disease. Several long-term prospective studies have shown that lowering serum cholesterol levels decreases the risk for coronary artery disease in the future. This has prompted a more aggressive approach to screening and therapy for hypercholesterolemia in young patients. The current recommendations for serum cholesterol screening include the child of a single parent with a cholesterol level greater than 240 mg/100 mL or if the history is unobtainable but there is a suspicion of hypercholesterolemia. The recommendations to perform a serum cholesterol level and lipoprotein analysis include children with parents or grandparents with a history of coronary angioplasty or coronary artery bypass surgery, men younger than 55 years of age, women younger than 65 years of age, and children with parents or grandparents with a documented myocardial infarction among men younger than 55 years of age or women younger than 65 years of age.
9.
(D)
Serum cholesterol levels can be measured in the nonfasting state anytime after the age of 2 years. If serum cholesterol levels are higher than 200 mg/dL, lipoprotein analysis is indicated. Lipoprotein analysis requires the patient to be fasting for 12 hours before the testing.
LDL = (total serum cholesterol) − (HDL)
− (triglyceride concentration × 0.2)
Low-density lipoprotein (LDL) levels <110 mg/dL, in the presence of elevated cholesterol levels, should be repeated in 5 years. If the LDL level is 110-129 mg/dL, a Step 1 diet is recommended. If the LDL level is higher than 130 mg/dL, then a Step 1 or Step 2 diet is recommended with consideration of medical therapy and further evaluation for secondary causes of hyperlipidemia.
10.
(D)
Secondary causes of hyperlipidemia include
• exogenous factors such as obesity, isotretinoin use, oral contraceptive use
• endocrine or metabolic diseases including hypothyroidism
• obstructive liver disease
• renal failure
• other factors including anorexia or a high-fat and high-cholesterol diet
11.
(B)
Familial combined hyperlipidemia is the most common etiology of inherited hyperlipidemias in children. It occurs with an incidence of approximately 1 in 300 individuals and is inherited in an autosomal dominant fashion. Laboratory analysis reveals elevation of cholesterol and/or elevation of triglyceride levels. The etiology of familial combined hyperlipidemia is a result of an increased apoB-100 production by the liver related to multiple genetic factors. The clinical course is characterized by late onset of coronary artery disease and peripheral vascular disease. Familial hypercholesterolemia occurs in approximately 1 in 500 individuals and is inherited in an autosomal codominant fashion. In the heterozygous form, there are elevated serum cholesterol levels and a high risk of premature coronary artery disease. The etiology of the hypercholesterolemia is a result of a decrease in the number of LDL receptors. In the homozygous form, there is severe hypercholesterolemia with increased risk of myocardial infarction. The etiology for hypercholesterolemia is nearly complete absence of LDL receptors. Mild hypertriglyceridemia is associated with obesity, glucose intolerance, hyperuricemia, and increased alcohol intake. Severe hypertriglyceridemia is a result of a deficiency of lipoprotein lipase and is associated with recurrent pancreatitis, hepatosplenomegaly, and xanthomas.
12.
(B)
In patients with hypercholesterolemia, therapy is not indicated for children younger than 2 years of age. In children older than 2 years of age, initial treatment includes the Step 1 diet recommended for approximately 3 months. If the serum cholesterol level remains elevated, then a Step 2 diet is recommended for 6-12 months. If the level continues to be elevated and the child is older than 10 years of age with an LDL higher than 190 or an LDL higher than 160 and a family history of hypercholesterolemia, then bile acid sequestrants such as cholestyramine are the first-line choice of medical therapy. In selected cases, lovastatin has been reported to be of beneficial use. However, it is currently not recommended for routine use.
13.
(A)
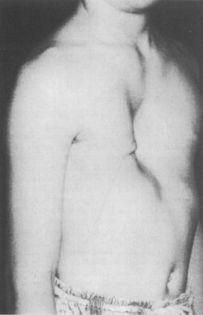
The patient in this scenario most likely carries the diagnosis of Marfan syndrome, an autosomal dominant genetic disorder due to a mutation in the fibrillin gene on chromosome 15. This leads to defective connective tissue disease. The clinical features include a long thin face, tall stature with the arm span greater than the height, pectus excavatum or carinatum, scoliosis, lens subluxation, and high arched palate (
Figure 5-1
). There is a family history of Marfan syndrome in 70-85% of cases. Patients with hypertrophic cardiomyopathy do not have the physical stigmata described in this case, but it is an important diagnosis in cases where there is a family history of sudden unexpected death. Patients with Turner syndrome have physical stigmata consistent with short stature and webbed neck; patients with Down syndrome also have short stature with characteristic facial features.