Pediatric Examination and Board Review (5 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

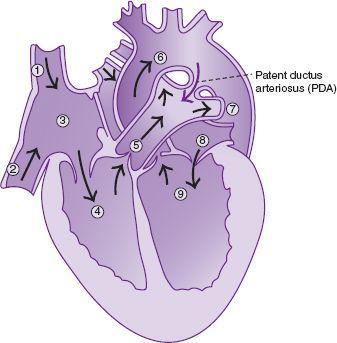
FIGURE 1-1
.
Patent ductus arteriosus (PDA). (1) Superior vena cava, (2) inferior vena cava, (3) right atrium, (4) right ventricle, (5) main pulmonary trunk, (6) aorta, (7) left pulmonary artery, (8) left atrium, (9) left ventricle.
2.
(D)
The ductus arteriosus in this neonate remains patent after 72 hours. The most appropriate test to confirm this is the echocardiogram. This test will not only confirm the diagnosis of the patent ductus arteriosus but will also assess any associated cardiac lesions. It is critical to check for pulmonary artery hypertension or ductal-dependent cardiac lesions when planning for closure of the patent ductus arteriosus.
3.
(D
) The presence of a small patent ductus arteriosus is unlikely to lead to significant left-to-right shunting or volume overloading and therefore does not place the child at risk for development of heart failure. There is about a 5% incidence of spontaneous closure of a small patent ductus arteriosus, and thus immediate surgery is usually not required in that situation. Recent review of subacute bacterial endocarditis has suggested that the lifelong risk for bacterial endarteritis with the presence of a patent ductus arteriosus is extremely low. Therefore, current guidelines do not recommend antibiotic prophylaxis for this condition.
4.
(B)
In this situation, a large patent ductus arteriosus has allowed significant left-to-right shunting resulting in pulmonary edema, shortness of breath, and left ventricular volume overload. The treatment options at this point include administration of indomethacin in an attempt to close the patent ductus arteriosus. Indomethacin is effective in approximately 80% of cases; however, its effectiveness decreases if administered after 2 weeks of age. Other treatment options for closure of a hemodynamically significant ductus arteriosus include surgery or transcatheter device closure. Both can be performed safely and effectively with minimal morbidity and mortality. Administration of oxygen to the patient with congestive heart failure because of a large leftto-right shunt would be detrimental in that it may decrease pulmonary vascular resistance and increase the degree of left-to-right shunting, exacerbating the symptoms of heart failure. The same is true for administration of nitric oxide in this situation. Administration of phenylephrine would cause an increase in systemic vascular resistance and result in a greater degree of left-to-right shunting.
5.
(A)
The etiology of shock in the neonate includes the following:
• hypoglycemia
• asphyxia
• sepsis
• intracranial bleeding
• arrhythmias including tachyarrhythmias and bradycardias
• cardiogenic shock because of left-sided obstructive lesions
• myocarditis
The least likely explanation of shock in this baby is asphyxia because there is no history of perinatal asphyxia or distress based on the birth history.
6.
(B)
Cardiogenic shock may be the first presentation in the neonate with congenital heart disease. Specific heart lesions causing left ventricular outflow tract obstruction may present in this manner. These lesions include critical aortic stenosis, hypoplastic left heart syndrome, and coarctation of the aorta. A patent ductus arteriosus allows for blood to bypass left-sided obstructions thus maintaining adequate cardiac output. With closure of the ductus, cardiac output is diminished. The neonate with cardiogenic shock from ductal-dependent lesions often presents at 1-2 weeks of age with shock related to the spontaneous closure of the ductus arteriosus.
7.
(D)
An echocardiogram would be the most useful test in this situation to determine if there is a ductaldependent cardiac lesion. It is also useful to detect primary myocardial dysfunction related to other causes of shock.
8.
(A)
The acute therapy for shock as a result of ductal-dependent cardiac lesions is infusion of prostaglandin E
1
in hopes of reestablishing patency of the ductus arteriosus.
9.
(E)
The other acute management strategies for shock in the neonate include inotropic support with dopamine or epinephrine, ventilatory support in cases of respiratory compromise, oxygen supplementation, and correction of metabolic abnormalities such as acidosis, hypokalemia, and hypocalcemia.
10.
(E)
Cyanosis can be divided into 2 clinical categories: central or peripheral. Central cyanosis is a result of a decrease in the oxygen saturation of blood supplying the body. Peripheral cyanosis is a benign finding caused by increased oxygen extraction in distal capillary beds and is commonly seen in normal neonates. The clinical detection of cyanosis occurs when approximately 3-5 g/dL of desaturated hemoglobin is present in the systemic circulation. The most common causes of central cyanosis in the neonate include cyanotic heart disease, hemoglobinopathies, and respiratory distress.
11.
(A)
The test most likely to help differentiate cyanotic heart disease from respiratory disease is the hyperoxia test. In this test, 100% oxygen is administered to the patient and the partial pressure of oxygen is measured. In patients with cyanotic heart disease, the partial pressure of oxygen rarely increases above the level of 100 mm Hg, whereas in lung disease there is usually some change from the baseline PO
2
with administration of oxygen. The lack of response to oxygen in cyanotic heart disease is a result of fixed right-to-left shunting of desaturated blood to the systemic circulation. Although the other tests mentioned may be helpful in the evaluation of the cyanotic neonate, they are not as sensitive in differentiating cardiac from respiratory etiologies.
12.
(A)
Cardiac lesions associated with cyanosis include
• transposition of the great arteries (the most common)
• tetralogy of Fallot
• truncus arteriosus
• tricuspid atresia
• pulmonary atresia
• total anomalous pulmonary venous return
Other lesions include single-ventricle physiology such as hypoplastic left heart syndrome, or Ebstein anomaly of the tricuspid valve with right-to-left shunting across an atrial septal defect.
13.
(A)
In patients with cyanosis because of heart disease, there is either obligate mixing of saturated and desaturated blood reaching the systemic circulation (eg, truncus arteriosus) or decreased effective pulmonary blood flow. In either situation, promotion of increased pulmonary blood flow or improved mixing of desaturated and saturated blood would increase the systemic oxygen saturation. This is acutely achieved by infusion of prostaglandin E
1
to reestablish (or maintain) patency of the ductus arteriosus. Therefore, in situations where cyanosis because of heart disease is suspected, infusion of prostaglandin E
1
should be instituted as soon as possible.
14.
(D)
Patients with tetralogy of Fallot are at risk for a hypercyanotic “tet” spell. This usually occurs in patients older than 2 years of age, although it has been reported at younger ages. The mechanism of a hypercyanotic spell is acute and progressive pulmonary stenosis, with increased right-to-left shunting of desaturated blood to the systemic circulation. This is precipitated by an increase in circulating catecholamines, anxiety, hypoxia, or dehydration. Interventions to break this cycle include administration of oxygen, morphine, propranolol, or phenylephrine, placing the child in a knee-chest position. In extreme cases, muscle relaxation and intubation are required. Rectal stimulation would serve to worsen the crisis by increasing the catecholamine levels (
Figure 1-2
).
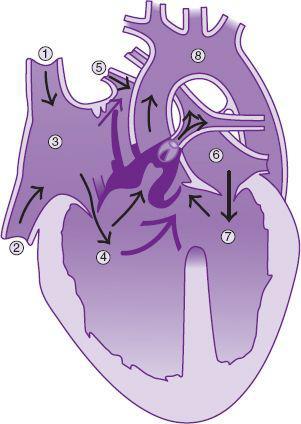
FIGURE 1-2.
Tetralogy of Fallot. There are infundibular and pulmonary stenoses. There is also right-to-left shunting at the atrial level. (1) Superior vena cava, (2) inferior vena cava, (3) right atrium, (4) right ventricle, (5) right pulmonary vein, (6) left atrium, (7) left ventricle, (8) aorta.
15.
(E)
Complications in patients with chronic cyanosis include polycythemia (compensation for decreased systemic oxygen tension), and risk of strokes because of an increased propensity for forming blood clots and increased blood viscosity. This is particularly concerning when the hematocrit is higher than 70%. A relative anemia may be seen in patients with cyanosis with low hemoglobin indexes. Some have suggested that this increases the risk of stroke because of increased blood viscosity. Another complication is brain abscess formation because of poor venous blood flow and increased susceptibility to infection. Impaired cognitive function is associated with long-standing cyanosis. The degree of impairment is related to both the degree and duration of cyanosis.
 S
S
UGGESTED
R
EADING
Allen HD, Driscoll DJ, Shaddy RE, Feltes TF, eds.
Moss and
Adams Heart Disease in Infants, Children and Adolescents.
7th ed. Philadelphia, PA: Williams and Wilkins; 2007.
Braunwald E, Zipes DP, Libbey P, eds.
Braunwald: Heart Disease: A Textbook of Cardiovascular Medicine.
7th ed. Philadelphia, PA: WB Saunders; 2004.
