Insomnia and Anxiety (Series in Anxiety and Related Disorders) (19 page)
Read Insomnia and Anxiety (Series in Anxiety and Related Disorders) Online
Authors: Jack D. Edinger Colleen E. Carney

most of the herbal compounds and supplements mentioned here so their use as
sleep aids cannot be recommended.
Melatonin
Unlike the other compounds mentioned, melatonin is a hormone that is produced
by the pineal gland and, thus, occurs naturally in the human body. Melatonin is
synthesized from serotonin and mostly is secreted at night. Typically, melatonin
concentration levels in the blood begin to rise around dusk, reach a peak during the
middle of the night, and then decrease around dawn. Melatonin seems to have influ-
ences on the endogenous circadian system that regulates the timing of sleep in the
24-h day. For this reason, melatonin has been used to alter the timing of the sleep–
wake schedule under such conditions as jet lag, or to reset the biological clock in
those who have marked endogenous delay in the timing of their sleep onset each
night. In applications to insomnia, some studies have shown that melatonin results in
self-reported improvements in sleep onset latency and general sleep quality, but its
effects on other self-reported sleep measures is more equivocal (Buysse et al., 2005).
In addition, some studies suggest that melatonin administration leads to objective
Over-the-Counter Medications, Herbal Remedies, and Alternative Treatments
69
improvements in sleep latency (Hughes, Sack, & Lewy, 1998; Zhdanova et al.,
2001). However, a recent comprehensive review of the melatonin literature suggested
that the research supporting the use of this agent as an insomnia remedy is of
questionable quality (Buscemi et al., 2004).
Currently, melatonin sold over-the-counter does not have an FDA-approved
indication for insomnia and, therefore, it is not regulated by the FDA. As such,
formulations sold to the general public are not standardized in their compositions.
However, the side effects associated with melatonin use appear to be minimal.
The most common side effect is headache. In rare cases, other side effects includ-
ing disorientation, nausea, seizures, and shortness of breath have been reported
(Buysse et al., 2005). Nonetheless, for most individuals, short-term use to address
insomnia is safe, but little data currently exist concerning its long-term effects.
Alcohol
Alcoholic beverages are widely used as a common home remedy for sleep difficul-
ties. In fact, it is estimated that as many as 30% of all chronic insomnia sufferers
use alcohol as a routine sleep aid (Ancoli-Israel & Roth, 1999). Alcohol is a CNS
depressant and, as such, has a relaxing and sleep-inducing effect, particularly on
anxious individuals. It tends to reduce sleep onset time and increase the amount of
nonrapid eye movement sleep (NREM) while reducing rapid eye movement sleep
(REM) during the initial half of the night (Gillin, Drummond, Clark, & Moore, 2005).
However, alcohol is metabolized very rapidly, typically at the rate of one glass of wine
or about 8 oz of beer for 1 h. After several drinks, alcohol is fully metabolized
by the body about halfway through the night resulting in shallow, broken sleep with
increased REM (dreaming) sleep in the latter portion of the night (Gillin et al., 2005).
In some individuals, sleep may be disrupted by stomach irritation, a full bladder,
rebound wakefulness, sweating, or nightmares. Thus, whereas alcohol often makes
it easier for the insomnia sufferer to fall asleep, sleep maintenance and overall sleep
quality are usually disrupted resulting in an overall compromise of the total
sleep period.
Alcohol has a number of side effects and risks associated with both its short- and
longer-term use. In the short run, alcohol tends to increase the likelihood of snoring
and apneic (i.e., breathing pauses) episodes even in those without any history of
sleep apnea (Dawson, Lehr, Bigby, & Mitler, 1993). If alcohol is used routinely,
tolerance usually develops resulting in the need for dose escalation to obtain con-
stant subjective effects. In addition, alcohol is associated with considerable risk for
dependence. If dependence does develop, the alcohol user typically reports diffi-
culty sleeping without a drink. With prolonged use of alcohol, daytime hypersom-
nolence and cognitive dysfunction may be observed. Individuals who develop
alcohol dependence often show marked sleep disruption upon becoming abstinent.
Moreover, heavy and long-term users often show continued disruption of sleep even
1–2 years after becoming abstinent (Brower, Aldrich, Robinson, Zucker, & Greden,
70
5 Medication Considerations
2001; Gillin et al., 2005). Thus, despite its popularity as a sleep aid, alcohol cannot
be recommended to address insomnia.
Can Common Anxiety Medications Cause Insomnia Symptoms?
Many individuals with anxiety disorders receive some form of pharmacotherapy as
treatment for their anxiety symptoms. Currently, the two classes of prescription
medications that are commonly used to treat anxiety disorders are the serotonin
reuptake inhibitors and the benzodiazepines. Included in the former group of com-
pounds are selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine,
paroxetine, sertraline, fluvoxamine, citalopram, and escitalopram. Also included in
this broad class of medications are the serotonin and norepinephrine reuptake
inhibitors (SNRIs) such as venlafaxine. Included in the latter class of medications
are such substances as diazepam, lorazepam, and clonazepam. As both of these
types of compounds can have effects on sleep or wakefulness, it is useful to con-
sider those effects here.
Whereas SSRIs and SNRIs are often considered the first line pharmacologic
agents prescribed for managing anxiety symptoms, these medications can have
negative effects on sleep and wakefulness. All of these medications may induce
insomnia. In fact, the rate of treatment-induced insomnia ranges from a low of
about 5% with escitalopram to as high as 22% with fluoxetine (Schweitzer, 2005).
Likewise, these medications may result in daytime sedation with such symptoms
occurring in 0–5% of all patients treated with escitalopram and slightly over 20%
of those treated with fluoxetine or paroxetine (Schweitzer, 2005). Thus, with
patients receiving an SSRI or SNRI report insomnia and/or over sedation in the
daytime, the possibility that such symptoms relate to their antianxiety agents should
be considered, particularly when such symptoms emerge after treatment initiation.
Benzodiazepines such as diazepam, lorazepam, and clonazepam are commonly
prescribed for the management of anxiety disorders. These medications may be
administered to manage daytime anxiety symptoms and/or at bedtime if insomnia
accompanies the anxiety symptoms. The benzodiazepines mentioned all have such
properties as tolerance and dependence with continued use (Greenblatt, 1992).
Generally, insomnia does not develop during periods of active use but may develop
upon abrupt withdrawal, particularly if such medications are typically taken at
bedtime to manage insomnia symptoms. This withdrawal effect is likely to be
most pronounced with lorazepam, given its short half-life, but insomnia may
develop upon withdrawal of the other medications mentioned as well (Greenblatt,
1991; Sironi, Miserocchi, & De Rui, 1984). Daytime sedation/drowsiness may
result from these medications with such effects being more likely and pronounced
with the longer acting agents (e.g., clonazepam) as opposed to the shorter acting
ones (e.g., lorazepam). Other side effects common to these agents include impaired
motor coordination, dizziness, impaired learning, anterograde amnesia, agitation,
and depression.
Combining Sleep Medications with CBT for Insomnia
71
Combining Sleep Medications with CBT for Insomnia
Sleep medications are so widely available and well publicized that many who seek
out cognitive behavioral insomnia therapy have either used such medications or at
least considered their use. As noted previously, many who begin CBT for their
insomnia present on one or a combination of sleep medications, both prescription
and over-the-counter preparations. These patients may ultimately want to discon-
tinue their sleep medications entirely but are not ready to do so at the time they
enter treatment. Others may not wish to stop using their medications at all but
desire additional nonmedicinal intervention for sleep. Usually, a strong psychologi-
cal dependence on sleep medications has developed and such individuals feel
unable to sleep without them (Belleville, Guay, Guay, & Morin, 2007; Lichstein
et al., 1999). Such individuals may overvalue the effectiveness of their sleep medi-
cations and lack confidence in their ability to sleep without them (Belleville et al.,
2007). Moreover, compared to insomnia sufferers without medication dependence,
there may be a greater degree of unhelpful beliefs about their insomnia and notable
pessimism about their ability to gain control over their sleep (Carney, Edinger,
Manber, Garson, & Segal, 2007). Given these observations, it seems reasonable to
assume that they could be relatively difficult to treat with strategies such as CBT.
Despite this concern, the data available tend to suggest that such people can and
do benefit from CBT for their insomnia problems. In fact, most studies that have
examined the relative responses of those who enter treatment on and off hypnotic
medications tend to show that hypnotic use does not necessarily dampen CBT treat-
ment response (see Morin et al. 2006 for recent review). Typical of such findings
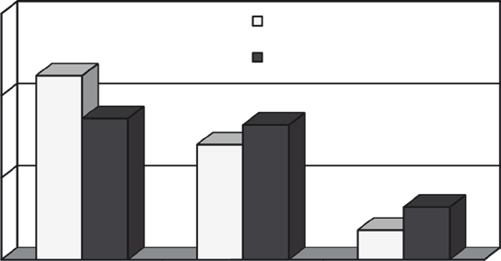
are the data shown in Fig. 5.1. These data derived from a large (
n
= 127) case repli-
cation series study (Verbeek, Schreuder, & Declerck, 1999) of those treated with
CBT showed no difference in the global treatment responses of hypnotic users and
nonusers. Similarly, in two large effectiveness studies, Espie (Espie, Inglis, Tessier,
& Harvey, 2001; Espie et al., 2007) found that patients who used hypnotics on a
chronic basis were no less likely to respond to a nurse-administered CBT insomnia
intervention delivered in primary care settings than were those patients who were
medication free. Although at least one small (
n
= 21) uncontrolled trial (Backhaus,
Hohagen, Voderholzer, & Riemann, 2001) suggested that medication-free patients
respond better to CBT than do those who are hypnotic dependent, this finding
appears contrary to most CBT studies that have conducted post-hoc comparisons of
such groups. Thus, given most current evidence, it seems that a history of hypnotic
medication use should not be considered as a contraindication or limiting factor
when considering people for insomnia treatment with CBT.
A slightly different set of considerations arises when determining whether hyp-
notic medications should be used in combination with CBT to enhance insomnia
treatment outcomes. Rationale for such a treatment combination derives from con-
sideration of the relative advantages and disadvantages of each of these two treat-
ment modalities. Hypnotic medication has the advantage of producing immediate
sleep improvements usually on the first night of administration. However, all hypnotic
72
5 Medication Considerations
Subjective Improvement Ratings
75
Medication Free n = 34
56
Hypnotic Users n = 49
50
ple
43
41
35
of sam% 25
16
9
0
Good Outcome
Reasonable
No Change
Outcome
Good Outcome
= improved sleep + improved daytime function +
able to cope with sleep problem
Reasonable
= Improvement in at least 1 of these 3 areas
No Change
= no perceived improvement
Fig. 5.1
Response of hypnotic users & nonusers to CBT (Verbeek et al., 1999)
agents carry some risk for at least psychological dependence with their long-term
