i bc27f85be50b71b1 (94 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

Spinal Injury Association (ASIA) Impairment Scale.31 This scale classifies SCI acccording to motor and sensory funcrion32: A Complete-No sensory or motor function is preserved in 54-5.
=
B
Incomplete-The preservation of sensory function without
=
motor function below the neurological level and includes 54-5.



3 1 0 ACUTE CARE HANDBOOK fOR PHYSICAL THERAI'ISTS
C
Incomplete-The preservation of motor function below the
=
neurological level. Muscle function of more than half of key muscles below this level is less than 3/5 .
D
Incomplete-The preservation of motor function below the
=
neurological level. Muscle function of at least half of key muscles
below this level is less than 3/5.
E Normal-Motor and sensory function are intact.
=
The most common types of incomplete SCI syndromes are
described in Table 4-1 9. The immediate physiologic effect of SCI is
spinal shock; the triad of hypotension, bradycardia, and hypothermia is secondary to altered sympathetic reflex activity." It is beyond the scope of this book to discuss in detail the physiologic sequelae of
SCI. However, other major physiologic effecrs of SCI include autonomic dysreflexia; orthostatic hypotension; impaired respiratory function; bladder, bowel, and sexual dysfunction; malnutrition;
stress ulcer; diabetes insipidus; syndrome of inappropriate secretion
of antidiuretic hormone; edema; and increased risk of deep venous
rhrombosis.
Clinical Tip
•
If, during physical therapy intervention, a patient
wirh SCI develops signs and symptoms associared wirh
autonomic dysreflexia, return the patient to a reclined
sitting position, and notify the nurse or physician
immediarely. Signs and symptoms of autonomic dysreflexia include headache, bradycardia, hypertension, and
diaphoresis ."
•
During rhe early mobilization of the patient with SCI
into the sitting position, consider using compression stockings or Ace wraps on the legs and an abdominal binder to
prevent or minimize orthostatic hypotension.
The management of SCI rypically includes medical srabilization
with ventilatory support (if indicated); immobilization of the spine
with a collar, orthosis, traction, halo vest, or surgical repair; methylpredisolone or other pharmacologic therapies; treatment of secondary injures; pain management; and psychosocial support.
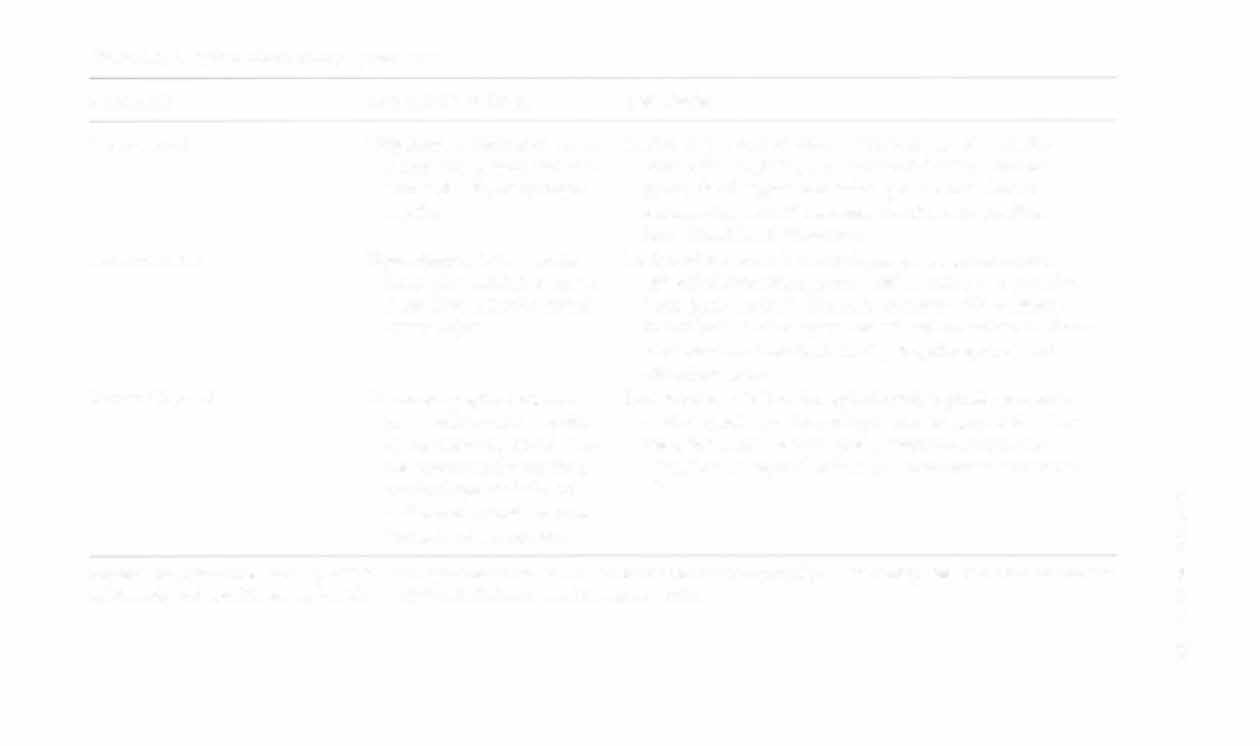
Table 4- 1 9. Spinal Cord Injury Syndromes
Syndrome
Mechanism of Injury
Description
Central cord
Hyperextension injury, or as
Lesion of the central cord exerts pressure on anterior
a result of tumor, rheumahorn cells. Typically presents with bilateral motor
toid arthritis, or syringoparalysis of upper extremities greater than lower
myelia
extremities, variable sensory deficits, and possible
boweUbladder dysfunction.
Anterior cord
Hyperflexion injury. acute
Lesion of the amerior cord damages the anterolateral
large disc herniation, or as
spinothalamic tract, cortical spinal tract, and anterior
a result of anterior spinal
horn (gray marrer). Typically presents with bilateral
artery injury
loss of pain and temperature sensa cion and motor function with rerained light touch, proprioception, and
vibracion sense.
Brown-Sequard
Penetrating spinal trauma
Lesion of one-half of the spinal cord; rypically presents
(e.g., stab wound), epiduwith conrralateral loss of pain and temperature sensaral hematoma. spinal artetion; ipsilateral loss of rouch, proprioception, and riovenous malformation,
vibration sensej and ipsilateral motOr paresis or paralycervical spondylosis, or
sis.
z
unilateral articular process
�
fracrure or dislocation
8
:;;
Sources: Data from DA Buckley, MM Guanci. Spinal cord trauma. Nurs Clin North Am 1999;34(3); and ]V Hickey (ed). The Clinical Pracrice
�
-<
of Neurological and Neurosurgical Nursing (4[h cd). Philadelphia: Lippincorr, 1997.
�
w
�
�

3 1 2 AClJTE CARE HANDBOOK FOR PIIYSI(;AL TI-IERAI'ISTS
Cerebrovascular Disease alld Disorders
A patent cerebral vasculature is imperative for the delivery of oxygen to
the brain. Alterations of the vascular supply or vascular Structures can
cause neurologic dysfunction from cerebral ischemia or infarction.
Transient Ischemic Attack
A T1A is characterized by the sudden onset of focal neurologic deficits, such as hemiparesis or altered speech secondary to cerebral, retinal, or cochlear ischemia, commonly from carotid or vertebrobasilar disease.34 These deficits last less than 24 hours without residual
effects. The management of TIAs involves observation, treatment of
causative factor (if possible), anticoagulation, and carotid endarterectomy. TIA is often a strong prognostic indicator of stroke.
Cerebrovascular Accident
A eVA, otherwise known as a stroke or brain attack, is characterized
by the sudden onset of focal neurologic deficits of more than 24
hours' duration secondary to insufficient oxygen delivery to the brain.
The most prominent risk factors for CVA include older age, male
gender, black race, hypertension, coronary artery disease, hyperlipidemia, atrial fibrillation, hypercoagulable srare, diaberes mellirus, obesity, smoking, and alcohol abuse.35
Ischemic CVA is rhe resulr of cerebral hypoperfusion. An ischemic
CVA has a slow onset and is due to thrombotic disease, such as carotid
artery stenosis or arteriosclerotic intracranial arteries, or an embolus
from the heart in the setting of atrial fibrillation, meningitis, prosthetic
valves, patent foramen ova Ie, or endocarditis. The management of
ischemic CVA involves blood pressure control (normal to elevated
range), treatment of causative factors (if possible), anticoagulation,
recombinant tPA,36 cerebral edema comrol, prophylaric anticonvulsant
therapy, and carotid endarterectomy (if indicated).
Clinical Tip
A patient who has received tPA is at risk for intracranial hemmorhage or bleeding from other sites and requires strict blood pressure control during the first 24 hours of infusion." Physical therapy is usually nor initiated during this time frame.