How to Become Smarter (66 page)

The symptoms of groups AB and BA will be evaluated every two weeks starting on the day immediately before the 10-week study. Depending on the available data regarding the standard deviation and the coefficient of reliability of the ADHD rating instrument in question, the required sample size for the clinical trial may be smaller or greater than forty patients. An example of sample size calculation is given below using hypothetical characteristics of a non-existing ADHD rating instrument. For instance, if the mean is assumed to be 12, standard deviation as 3.6 (30%), and the reliability coefficient of the instrument as 0.7, then the required sample size to detect an effect size equal to one half of standard deviation will be 78 participants total, or 39 patients in each group according to the PASS software [
633
]. The settings in the PASS program are as follows: menu “Means,” “Two means,” “2x2 cross-over designs,” “Inequality tests using differences.” The following parameters should be set: Find (solve for) = sample size; Alpha = 0.05; Power(1 – beta) = 0.8; Diff0 = 0; Diff1 = 1.8; Sd = Std Dev of Differences = 2.79; Alternative hypothesis = two-tailed T test.
According to the paper by Jacobson and Truax [
634
], standard deviation of the expected mean (treatment group) can be estimated as approximately equal to standard deviation of the variable prior to treatment, while standard deviation of the differences S
dd
(used in sample size calculations for crossover trials) can be estimated as
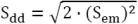
where standard error of the mean S
em
is estimated as
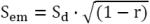
where S
d
is standard deviation of the variable in the group of patients before treatment and
r
is a reliability coefficient of the ADHD rating instrument [
634
].
In addition, groups AB and BA can be tested for sustained attention once a week starting on the day immediately before the 10-week study. For this purpose, it is possible to use a continuous performance test such as the Test of Variables of Attention [
635
-
638
].
The PASS software [
633
] can also calculate the sample size for a different type of study: a crossover equivalency study, where the controls will receive psychostimulant medication. This study can compare the effectiveness of the modified high-protein diet to that of psychostimulant medication. In principle, the dietary and pharmacological approaches are not mutually exclusive and can be combined if necessary.
Finally, the modified protein supplement or the modified high-protein diet can also be tested for their potential benefits for knowledge workers. It would be safe to test this approach for four weeks, with the same exclusion criteria and study design as described above for the ADHD trial. The main expected benefit is the ability to concentrate on reading or writing for several hours at a time. Tests of sustained attention usually take 10 to 20 minutes and will not be useful for this purpose. A test of “attentional stamina” will need to be devised that assesses the ability to maintain the focus of one’s attention on an object (e.g., a simple text) for 3 hours. This task should require neither advanced knowledge nor fluid intelligence. A moving band of text on a computer screen is a good candidate. A distraction will cause irreversible loss of information. An additional method of testing is the self-rating questionnaire (Reading/Writing Productivity Questionnaire) provided in
Appendix V
.
(for biomedical researchers)
Existing evidence of antianxiety effects of moderate heating of the body
(L
AY
L
ANGUAGE
S
UMMARY
): see the
main text
.
Several studies support this idea [
353
,
817
,
818
,
894
]. Exposure to moderate heat can increase the level of GABA (gamma-amino-butyric acid) [
639
,
640
] and serotonin in the brain [
641
,
642
], chemicals that have sedative properties. Intracerebroventricular injection of serotonin and GABA (separately) reduces activity of laboratory rodents, which is suggestive of sedative effects [
643
,
644
]. Consumption of tryptophan, the metabolic precursor of serotonin, by human subjects causes sleepiness [
645
]. SSRIs, which increase the extracellular level of serotonin in the brain, typically reduce activity of laboratory rodents and improve symptoms of anxiety in patients after 2 or 3 weeks of daily administration [
450
]. The effects on cerebral GABA and serotonin may explain the sedative effects of heat, such as slowing of mental processes [
352
]. The increased level of serotonin in the brain may explain heat-induced fatigue according to the serotonin hypothesis of central fatigue [
646
]. Another possible explanation for the sedative effect of warming involves hypothalamus. Skin warming activates neurons in the preoptic and anterior hypothalamus, the brain regions participating in the control of the circadian clock [
348
].
The increased level of GABA in the brain and the depressant effect of moderate heating, suggest that this treatment may have an anxiolytic effect. Known anxiolytics such as benzodiazepines and barbiturates enhance activity of GABA receptors and a recent study showed that valproate (a drug that increases the extracellular level of GABA in the brain [
647
]) is beneficial in anxiety [
648
]. It may seem self-contradictory that this book is also trying to prove that moderate cooling of the body has anxiolytic effects too.
S
This is not necessarily a contradiction, since treatments with the opposite mode of action are effective in depression (SSRIs and tianeptine), and these same treatments also have anxiolytic properties [
450
,
649
], even though SSRIs usually have a sedative effect, whereas tianeptine has a mild activating effect [
391
,
650
]. Additionally, both heating and cooling can relieve physical pain, despite the opposite mode of action [
412
]. It is possible that one these treatments (cooling or heating of the body) or both can trigger panic attacks in some patients with anxiety disorders; further research is needed.
As for practical application of heat, there are two possible types of treatment: a continuously hot environment, 29-30°C, and brief sessions of hot hydrotherapy (baths or head-out showers at 38-40°C, 5-10 minutes). Neither treatment should raise the core body temperature by more than 0.5°C. My self-experimentation suggests that the second approach (hydrotherapy) causes fluctuations of the activity level; namely, slight fatigue and relaxation after the procedure are followed by overactivity several hours later. The hot environment does not cause significant fluctuations of the activity level, although it reduces activity while the treatment is ongoing. Another difference between these two treatments is that the hot environment tends to lower normal mood and has little or no effect on low mood, whereas hot hydrotherapy (without hyperthermia) improves low mood and causes a slight elevation of normal mood. Based on these unpublished observations, it is possible that brief sessions of moderately hot hydrotherapy are more effective at reducing anxiety compared to a hot environment.
There are reports in literature which show that body heating can lower normal mood [
352
,
651
], but can improve depressed mood [
356
]. This is suggestive of a mood stabilizing effect, which may have to do with the heat-induced increase of the level of GABA in the brain. Valproate is a drug that can increase extracellular GABA concentration in the brain, and the FDA has approved it as a mood-stabilizing medication for bipolar disorder [
647
]. My own unpublished observations suggest that hot showers or hot baths (without hyperthermia) are beneficial if mood is mildly depressed; however, these treatments are extremely uncomfortable if mood is significantly depressed. In the latter case, a thermoneutral or tepid shower (5-10 minutes) followed by an adapted cold shower are beneficial. If elevated mood has to be lowered, a constantly hot environment is effective, but hot hydrotherapy is not helpful: it has a brief beneficial effect (2-3 hours, if core body temperature rises above 38°C) followed by a swing in the opposite direction.
(for biomedical researchers)
Theoretical evidence of neuroleptic effects of hyperthermia
(L
AY
L
ANGUAGE
S
UMMARY
): Heat can suppress dopamine activity in the brain, lower mood, and promote lethargy and a loss of interest. These effects are similar to those of antipsychotic drugs. In addition, increased body temperature causes disabling fatigue, which can be helpful in the treatment of severe agitation. The section describes a possible procedure that involves daily immersion in hot water. Possible side effects include skin irritation and suppression of some components of the immune system.
Patients who are reading these lines should not experiment with hyperthermia because it carries a risk of serious side effects, especially when combined with neuroleptic medication. Clinical effectiveness of hyperthermic treatments in psychosis is currently unknown.
- Hyperthermia (increased core body temperature) increases the level of serotonin and serotonergic activity in the brain as evidenced by an elevated plasma prolactin in humans [
354
] and direct measurements in the brain of laboratory animals [
641
,
642
]. The plasma level of prolactin is positively regulated by serotonergic neurons and negatively regulated by dopaminergic neurons [
355
,
652
]. Serotonergic neurons mostly have inhibitory projections to dopaminergic neurons in the mesolimbic system [
653
]. Inhibition of dopaminergic activity in the brain may be beneficial in psychosis because it is thought that psychosis is associated with hyperfunction of the dopaminergic system (according to the dopamine hypothesis of schizophrenia). - Dopaminergic neurons serve many functions and some of them directly control mood (dopamine reuptake inhibitors typically elevate mood within 30 minutes [
458
,
459
], whereas dopamine antagonists depress mood within hours [
460
,
461
]). This can explain the immediate dysphoric effect of exposure to heat reported in several studies [
352
,
651
] because this treatment inhibits dopamine activity in the brain. The mood recovers quickly after exposure to heat is discontinued (within 30 to 60 minutes) [
352
,
651
]. - Similarly, neuroleptic drugs lower mood [
460
,
461
] and inhibit dopaminergic activity in the brain; they can also cause hyperprolactinemia [
355
,
652
]. Incidentally, neuroleptic drugs can affect thermoregulation, and the rare side effect is neuroleptic malignant syndrome, which often manifests itself as hyperthermia. - Neuroleptic drugs used to be known as “major tranquilizers,” which implies that they can tranquilize the most violent and agitated patients. Similarly, hyperthermia may also be effective as a “major tranquilizer” because sufficiently high core body temperature (39°C or higher) can depress electrical activity of the cortex [
819
,
820
] and cause disabling fatigue [
654
,
655
].
