Extreme Medicine (4 page)
Authors: M.D. Kevin Fong

The electrical activity in Esmail's brain is, at this point, undetectable. He is not breathing and has no pulse. Physically and biochemically he is indistinguishable from someone who is dead. It seems impossible to believe that he might be successfully resuscitated from this state and go on to be the man he was before.
Yet after thirty-two minutes, the repair is complete and Dr. Elefteriades is ready to reestablish Esmail's circulation. The team warms his freezing body, and very quickly his heart explodes back into life, pumping beautifully, delivering a fresh supply of oxygen to Esmail's brain for the first time in over half an hour.
A day later, I visit Esmail on the intensive-care unit. He is awake and well, even if he's in a little pain, and his wife stands by his bed, overjoyed to have him back.
To cure this man, his surgeons had to come close to killing himâusing profound hypothermia to buy his survival. Esmail is living proof that physical extremes can cure as well as kill.
â
T
HERE IS ANOTHER EXTREME
that we have recently begun to explore, defined not by environmental conditions, like Scott's Antarctica, but by disease and injury. Modern intensive-care medicine hangs ordinary people out at the very limits of endurance, to endure perilous derangements in physiology, with the expectation that they might survive and go on to lead normal lives. Life at the extremes can be lifesaving.
Evolution did not prepare us for life at the extremes. Only engineering and technology allow us to cheat our environment and our biological fateâand then only temporarily. One of the questions this book will address is whether technology emboldens us before we understand its consequences. Think again of that medical team heating Anna BÃ¥genholm's chilled blood and pumping it back into her body, with only the slimmest hope that she would survive to lead a normal life. Perhaps we have no business pushing the envelope after all. Perhaps we have finally gone too far.
But Anna did make a complete recovery. She owes her life to science, technology, and medicine and to an understanding of the biology of deep hypothermia that is as young as she is. So goes the story of our exploration of the extreme tolerances of the human body. It is a story of tragic loss and outrageous survival, of questions about life and death and an attempt to understand what lies in between.
Within a century, we have come to understand the process that killed Scott. More than that, we overcame it and learned to use it to our advantage in medicine. The intervening decadesâbetween Scott's heroic death and Anna BÃ¥genholm's remarkable survivalâsaw progress in the field of medicine unparalleled in any other century. Flying ambulances, systems for the advanced management of traumatic injuries, the artificial cocoon of intensive care, techniques to bypass and replace the function of the human heartâall of these were necessary to allow Anna to survive an insult that Scott could not. But each of those innovations arose by accident, the products of other, unrelated challenges. There was no grand scheme through which we arrived at this point in history with such high expectations of life and its survival. In medicine and physical exploration, we moved forward into the unknown always hopeful that good fortune and survival lay in store.
â
I
N THE END,
S
COTT'S EXPLORATION
aboard the
Terra Nova
wasn't in vain either. The expedition that he led wasn't the first to reach the South Pole, but it was one with an important scientific legacy. It laid the foundations for the discipline of glaciology and found fossil specimens that would later point to an incredible truth: The southern continents of the world had once been linked together as a single landmass. The penguin skins collected by Scott's companions Apsley Cherry-Garrard, Edward Wilson, and Henry Bowers on their infamous “worst journey in the world,” a trek across the Ross Ice Shelf to a penguin rookery, provided a benchmark sample that would later help scientists establish the persistence and bioconcentration of DDT insecticide after its introduction into the global food chain in the twentieth century.
Scott's exploits aboard the
Terra Nova
were to have been the crowning glory of a triumvirate of expeditions that included Scott's first voyage to Antarctica aboard the
Discovery
in 1902 and Shackleton's
Nimrod
expedition in 1907âendeavors that were instrumental in opening up the continent of Antarctica to science. Scott may have died, but what he and his expedition team started at the turn of the
twentieth century in time became a wider program of scientific research, one of fundamental importance.
By the middle of the century, the scientific survey teams of several nations had established a plethora of permanently manned bases in Antarctica. In 1985, observations by the British Antarctic Survey detected the thinning of the Earth's ozone layer around the South Polar region: the so-called ozone hole. Ozone in our atmosphere absorbs ultraviolet radiation, protecting us from its harmful effects. This discovery and the later realization that ozone depletion was being catalyzed by halogen atoms in chlorofluorocarbons (CFCs) led to an international ban on these substances.
By the end of the century, these multinational scientific efforts in Antarctica delivered some of the most convincing evidence that global warming is a real phenomenon. Scott's race to the South Pole began as an exploratory effort into the unknown for which he paid with his life and the lives of his core team. However, the legacies of Scott's exploration are discoveries that might one day save our entire planet.
That is the truth of all explorationâin science or the physical world. We do not climb mountains, traipse to polar ice caps, split atoms, or unravel genomes simply because “they are there” but because we know that it is within the unanticipated fruits of exploration that our improved survival lies.
Scott's expedition marked the beginning of the end of the so-called Heroic Age of exploration. The Victorian concept of risking all for honor and the greater glory of God and country was cast into sharp relief by the catastrophe of the Great War. A new era of exploration was born, one that relied less upon the mettle of men and more upon the systems of protection that we were able to engineer to protect them. It is worth noting that after Scott and Amundsen's parties first arrived at the South Pole in 1912, no human set foot there again until 1956. And when they did, they arrived not in sleds driven by ponies or dogs but in aircraft.
â
T
ORVIND,
A
NNA, AND
I are walking along Mortimer Street; they have been lecturing about their experiences to an audience of doctors at the Royal Society of Medicine in London. They feel that this retelling of the story is important to change people's practice and expectations in the face of such extreme hypothermia.
There is a question I must ask Anna. If she'd had the choice at the time of her resuscitation at Tromsøâgiven the extraordinarily long period for which her heart had been arrested, knowing that the overwhelmingly likely outcome would have been death or a lifetime of disabilityâwould she have chosen to let the team proceed?
“Yes,” she tells me after a short pause, “because you never know.”
We continue our stroll through London. There is a point where water is rushing from what looks like a burst water main, flowing across the paving stones. Anna quickens her pace, breaking into a jog. For a moment, I wonder if this is one of those unexpected aversions that develop after a traumatic event. She was, after all, trapped under the ice, sinking into running water. Torvind says nothing. Perhaps it's something he's seen before. I am intrigued, briefly horrified, that this might be a sign of vulnerability or weakness.
I am still pondering this when a taxi runs through the sizable puddle that has collected in the gutter, drenching my feet and trousers. And I realize that, after she was entombed and frozen in an Arctic stream and endured the lowest recorded temperature of any cardiac arrest survivor in medical history, the only reason Anna's running is because she's smarter than me.
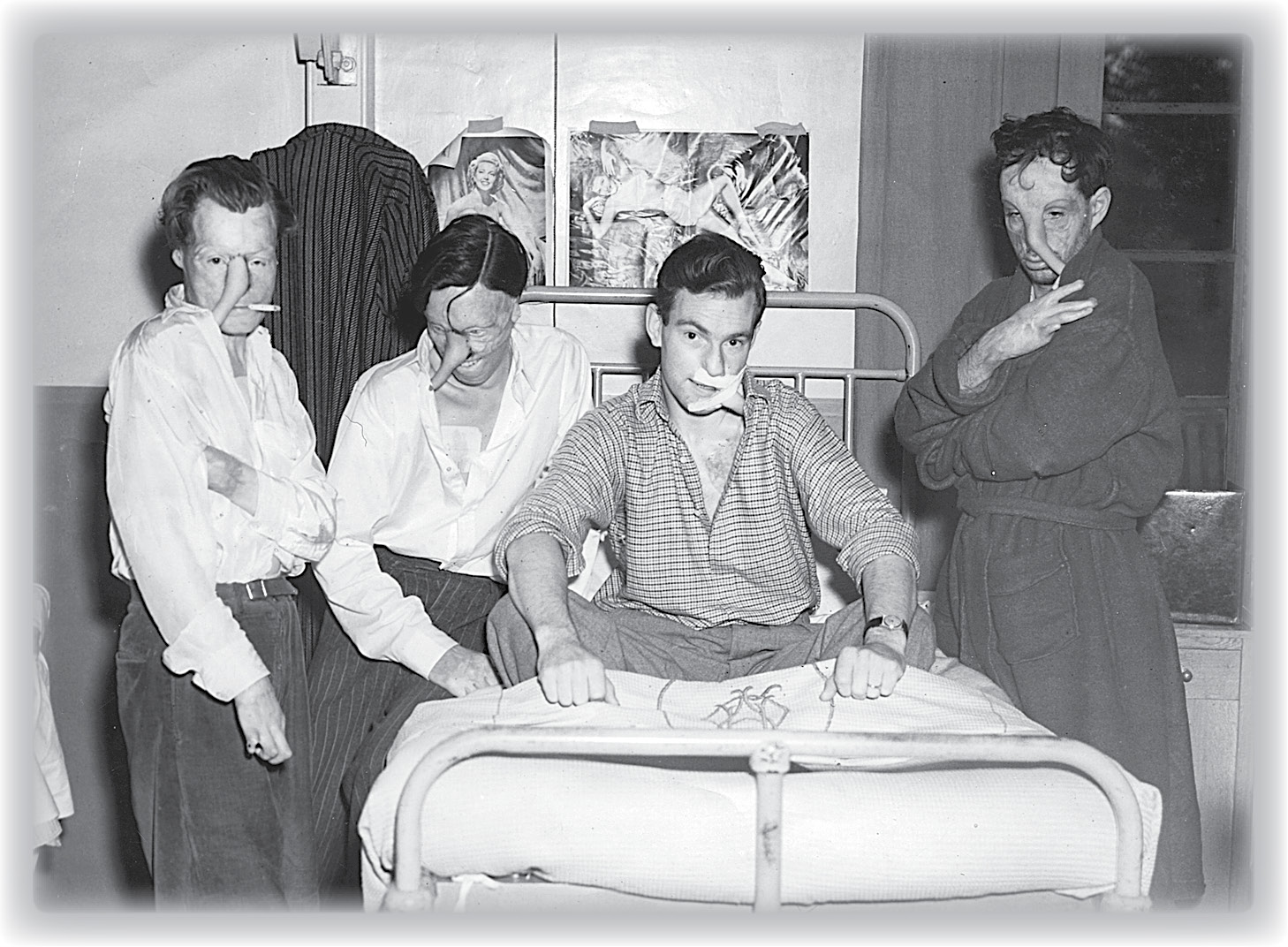
Second World War burn victims at the Queen Victoria Hospital in East Grinstead. The strips of flesh used for surgical reconstruction of their faces were kept alive by anchoring them to blood supplies at two locations. For these men the skin was bridged to the face from the forearm or chest.
(Reproduced by kind permission of the Guinea Pig Club)
H
ow much of that has to go in the vehicle?” asks the pilot, pointing at the mass of tubes, cables, monitors, and machines that surround my patient.
“All of it,” I tell him. The intensive-care side room looks cramped. Its contents must somehow be transferred to the roof of the hospital and crammed into the back of a medical-evacuation helicopter.
The pilot sucks air through his teeth, doing the mental arithmetic. It's a warm day; the air is thin. His engines can generate only so much lift. The more weight we have to carry, the shorter the range of the helicopter and the more hazardous the takeoff.
“How much has to be in the cabin with us?” he asks.
“All of it,” I repeat.
More air-sucking sounds.
“How much do you weigh?” he asks, looking me up and down.
“About 155 pounds,” I tell him.
“How about her?” he says, nodding indelicately at the nurse.
The man in the bed before us was caught in a house fire and is badly burned. The trauma team estimates that perhaps the full thickness of skin over as much as 50 percent of his body has been destroyed by fire, though it's hard to be sure. Underneath the char and the blisters, it is difficult to know what remains viable. Time is ticking by. Keeping him stable has taken all our efforts, and we are at the end of what we can offer here in this general intensive care ward. To give him the best chance of survival, he needs to be moved to a specialized burn unit.
We pour fluid into his veins, trying to keep up with the massive evaporative losses caused by the absence of skin cover. Protein is leaking from his vessels into his tissues; the osmotic pressure is taking more fluid with it. The alveoli of his lungs are filling as a protein-rich slushâleaking from his blood vesselsâexudes into them. Those tiny, all-important sacsâwhich allow air to be brought into contact with blood and oxygen to be exchanged for carbon dioxideâare becoming waterlogged. Things will get worse before they get better. We must move now. Tomorrow he may be too sick. But the closest specialist bed is more than two hundred miles away, too far for a safe road transfer. We'll need an aircraft. That's why the helicopter pilot is here, still doing sums in his head, weighing benefit against risk, as the patient slowly drowns in his own juices.
â
W
E DO NOT THINK OF SKIN
as an organ in the conventional sense. It lacks the solidity and the discrete locus of the more familiar viscera. That elastic but porous covering stretched over your frame, folds of flesh and imperfections that you know well enough to take for granted, fulfills an essential task. It is no less important to your continued survival than a heart or a pair of lungs.
It is tempting to think of skin as if it were simply a barrier, a line of separation between you and the world outside, a convenient way of preventing your viscera and tissues from sloshing about in an unsightly way.
It does indeed protect, but as a description of purpose and function, that is the grossest of understatements. It does much more than act as a bulwark against the abrasive world outside: It is the first line of defense against the microbial hordes massing on its surface; it prevents the excessive evaporation of the body's precious fluids; it harbors an exquisitely sensitive array of detectors that warn us of harm and allow us to respond fast enough to avoid further injury; and it thermoregulates to keep us warm when it is cold or cool us down when it is hot.
Skin is deeper than you think; in some areas of the body it is up to a fifth of an inch thick. The stuff at the top is dead, a keratinized layer that serves the purpose of physical protection. Below that layer is living, moist tissue that needs nutrients and a blood supply and is vulnerable to attack and injury.
If you take a microfine slice vertically through skin and examine it under a microscope, you can see the cellular structure of its layers. The specimens must be stained, otherwise the cells are largely clear and colorless. This is histology, the study of the microscopic anatomy of cells and tissues.
In my first year at medical school, I spent many hours staring into microscopes, trying to make sense of what appeared to be little more than washes of pink and purple abstract art. At the end of the course, we were supposed to be able to identify any number of organs and tissues from their microscopic appearance alone. It was like trying to identify different nations from close-up, unlabeled photographs of their fields and pavements. Sitting in long rows along laboratory benches stacked with microscopes, we strained our eyes to link the lecturer's elegant verbal descriptions to the purple mess visible through the eyepiece. Some of the slide material was pink with wavy strands, like streaky bacon, and we were assured that this was a perfectly acceptable descriptive term for that tissue. In time, and with a little help, the underlying structure began to make senseâthough not to everybody. One of my colleagues famously failed the first-year, one-hour histology exam, having written only the desperate words “It
all
looks like bacon to me!”
When you finally get your bearings, you can see that the skin is organized into distinct strata. The topmost layer, the epidermis, forms the tough barrier with which we feel so familiar. The cells of the epidermis are densely packed and further subdivided into layers. The base layer consists of stem cells that boast large purple-staining nuclei. These cells mature, eventually losing their nuclei and acquiring filaments of keratin, making them more rigid. As they develop, they ascend through the epidermal layer toward the surface, finishing at the top to form a tough protective layer of dead cells.
That layer tends to reinforce our image of the epidermis as a durable but passive barrier to the outside world. Yet it is anything but passive. The layers of epidermal cells, constantly being born and marching forward, are like a never-ending conveyor belt of foot soldiers throwing themselves at the wire. They mount a spirited defense: They create a dry and acidic environment hostile to bacterial growth; their tentaclelike appendages seek out and destroy foreign bacterial cells, and they secrete enzymes and fatty chemicals to further deter would-be colonists. The fight at the surface is fierceâa war against perpetual mechanical, chemical, and biological attack. Consequently the rate of attrition among these cells is high. For a single epidermal cell, that journeyâfrom birth in the basal layer to combat maturity on the surface of the epidermisâtakes something like six weeks. The rate of replacement must match the rate of loss, and the entire epidermal layer turns over every forty-eight days.
But the epidermis, the layer that we casually refer to as our skin, represents only what we can see. The epidermal layer is relatively uniform in appearance: stacks of purple-staining polyhedral cells topped by a paler weave of pink. Beneath this there is the dermis, which under the microscope looks like a vertical section through a chaotically planted vegetable garden. There are microscopic structures here that look like the cut surfaces of onions. That baconlike connective tissue is found here, dotted with strange-looking whorls, blood vessels, and tubes. Here the skin becomes more recognizable as an organ, run through with a network of glands and vessels and studded with organelles. It is from this layer that the skin derives both its elasticity and its supply of blood and nourishment.
Together the epidermis and dermis form a waterproof but breathable layer. They have pores that are small enough to prevent ingress of water droplets but large enough to let molecules of water vapor out. Gore-Tex clothing attempts to do the same thing, but as a breathable and waterproof barrier, it achieves only the very palest imitation of skin.
But it is the sensory array that is perhaps the skin's most remarkable feature. Able to resolve point contacts little more than a millimeter apart, it's capable not only of registering heat and cold but also of differentiating between a lover's caress and pain from a needle tip. Your skin is honed to provide a series of ever changing inputs in response to the cruel world outside, and these inputs shape your behavior in such a fundamental way that you are barely aware of the process.
That holiday in the sun that you seek, the sensation of warmth on your skin, is in part a product of the pattern of receptors that activate in response to incident radiation. Think of summer; think of winter; think of plunging headlong into a pool of water. Chances are that the first thing that enters your mind is that inexpressible pattern of skin receptor activation that we interpret as warmth, cold, or wetness.
The clothes that you are wearing right now are in part chosen because of the way they feel on your body. The receptors in your skin help you decide to move away from drafts, cause you to retreat from the roar of the fire, or urge you to get out of a chilly pool of water. Few sights, odors, or sounds could compel you to behave quite so urgently.
Consider this finely tuned early-warning system linked to a consciousness that understands both luxurious pleasure and intense pain. Then imagine setting it on fire.
â
T
HOUGH PAINFUL,
superficial burns involving only the epidermis are little more than that. Reddened by the dilation of blood vessels beneath and the inflammation of the tissues, they are rapidly healed and restored by the perpetual marching of those regenerating epidermal cells.
Even burns that extend below, into the upper two thirds of the dermis, retain the ability to heal and cover with new skin. A patch injured in this way generates islands of new epidermal cells that spread and eventually coalesce, replacing what was lost. These burns leave the bulk of the sensory architecture intact and are exquisitely painful. Damage to the tissue around pain receptors leaves them constantly firing. Inflammationâthe process that marshals cells of the body's defenses to fight infection and deal with injuryâretunes the pain receptors, making them hypersensitive. The same process brings fluid into the wound, which produces the blistered, weeping appearance, separating healthy tissue from that which is dead or irreversibly injured.
It takes great effort to survive a serious burn. Certainly they are among the most formidable injuries to manage in emergency medicine. After determined and skillful resuscitation, specialist burn treatment must follow. This care is complex. In addition to repairing and replacing damaged skin, it must also accomplish the difficult task of compensating for the failure of an essential organ.
â
T
HE MAN WE ARE TRYING
to cram into the back of that helicopter has already been the object of frenzied medical attention.
Burned larynxes can swell and occlude; smoke inhalation can prevent the lungs from exchanging oxygen and carbon dioxide; and poisonous gasesâcarbon monoxide and fumes from burning furniture and building materialsâcan asphyxiate. All of these will kill victims of fires in minutes or even seconds, long before the consequences of any external burn injury can manifest.
Yet if the opening minutes of the injury can be survived, the damage to the skin leaves a formidable constellation of problems. The vapor barrier function is lost, and the body's water evaporates uncontrollably from denuded body surfaces at a rate that is difficult to anticipate intuitively. The losses are both invisible and incredibly rapid. Without the cover of skin, your body dehydrates as surely as a wet sponge left out in the sun. And the burn itself triggers a severe inflammatory response in the body, compromising the integrity of the blood vessels, making them more porous and permeable, letting them spill fluid into surrounding tissues.
Such is the severity of this reaction that at the start of the twentieth century, victims with as little as 10 to 20 percent full-thickness burns over the surface area of their body would often die.
Thankfully, that has changed, but when it comes to burns, the extent of the surface area involved remains one of the key prognostic indicators. In the care of burns, we were taught a rule of thumb: the percentage area of body involved in a full-thickness burn plus the age of the patient gave the percentage chance that the patient would not survive. A sixty-year-old man with full-thickness burns over 40 percent of his body, for example, would not be expected to live. Today that is an outmoded concept; older people with more extensive burns are surviving against expectations, due in large part to the efforts of specialist burn units and the hard-won lessons of the twentieth century. Aggressive resuscitation with fluids, trauma systems, and early transfer to specialist units all helped to improve survival rates.
But in 1940 the medical fraternity knew little or nothing of all of this. For a pioneering generation of RAF fighter pilots, immolation was a risk they took every time they climbed into the cockpit. It's their experiences that have shapedâand continue to shapeâthe scope and ambition of burn treatments to this day.
â
O
N
A
UGUST 31, 1940,
the Battle of Britain was reaching a critical phase. The Luftwaffe was mercilessly bombing the Royal Air Force's airfields. Fighter Command was losing aircraft faster than they could be replaced, and the remaining pilots were fatigued. Throughout the south of England, fighter squadrons had scrambled time and time again to meet waves of German bombers escorted by Messerschmitt fighter planes. In the heat of that combat, the air was full of glowing munitions and crisscrossing aircraft. At RAF Kenley, on the outskirts of South London, thirty-two-year-old Tom Gleave had taken over command of 253 Squadron from Harold Morley Starr, who had been killed the previous day. Despite the ever-present danger, Gleave still found it impossible not to be captivated by the spectacle of the world as seen from the air. Scrambling from Kenley that day, he climbed quickly into a perfectly blue sky and dazzling sunlight. North of him lay the River Thames, glittering as it snaked its way through the London sprawl; to his south he could make out the Kent coastline shimmering in the summer haze. Below, unfurling at hundreds of miles an hour, rolled the patchwork quilt of the English Home Counties.
