Extreme Medicine (13 page)
Authors: M.D. Kevin Fong

Today, for the patients who arrive in our trauma units, we can do a lot more: We fill them with blood, splint limbs, throw stitches in the ruptured vessels we can see, scoop out bleeding spleens, repair punctured viscera, and pack lacerated livers. All this we do while holding their physiology stable with drugs and life-support machines.
Innovation in the pursuit of survival has taken us further still. We use beautifully nuanced physics to image, in fascinating detail, what remains hidden. We can thread long tubes into vessels, snaking them up from distant points of entry. We deploy devices that block or stent torrentially bleeding arteries and veins that can't be reached safely or quickly with a knife.
Once the patient has been taken from the scene of the accident and resuscitated, opened up, and the hemorrhage stopped, the fight continues. It's not enough to understand the mechanisms of bleeding vessels, crushed viscera, and fractured limbs. The bleeding taps having been turned off, limbs and organs having been saved, patients can still continue to decline.
In the most severely injured patients, kidneys can shut down, hearts can malfunction, and lungs can fail. It is this secondary wave of illness that follows in the wake of major injury that takes trauma out of the realm of the simple, physical disruption of a mechanism and turns it into a complex and formidable disease.
â
W
HY DO YOU BLEED TO DEATH?
That's the sort of seemingly innocuous question they dish out at finals. But it's like someone asking you how a wheel works. You think about it for about ten seconds, and then realize two things: You don't know and you never knew. If there's no blood running in your veins, you die. Yes, but death, or at least cardiac arrest, happens long before the system is empty of blood. So the question becomes what causes the cardiac arrest. That innocent question rests on determining what is behind the force and energy of every heartbeat. And then you know you're in trouble.
Nerves running from the brain send impulses to the heart, moderating its pace and force of contraction, and at times of stress, adrenaline circulates in the bloodstream, driving it harder and faster. But in the face of injury and massive blood loss, it's not the malfunction of this system that causes the heart to falter and stop. It is the mechanism of the heart itself. The heart has specialized muscle fibers that match the force of their contraction to the amount of blood entering it. If more blood returns to the heart just before the start of a heartbeat, the muscle contracts harder and so pushes out a larger volume. It's a way of making sure that the heart ejects the same volume of blood as enters it. If it were unable to match its ins and outs in this way, it would rapidly balloon and fail.
But when less blood returns to the heart, it beats with less force. And if the circulation is suddenly losing volume because of a hemorrhage, the heart empties further and its contractions become weaker. If bleeding continues unchecked, the heart eventually arrests.
In the first moments of treating a trauma victim, you're trying to prevent exactly that. It's why it's so important to stop the bleeding and maintain an adequate circulating volume in the blood vessels. Once the first phase of resuscitation is complete, after you've followed James K. Styner's all-important ATLS alphabet to the letter, much of your effort continues to be dedicated to the same task, stopping hidden bleeding with surgery and restoring volume with blood and fluids.
But even without resuscitation, the body starts to protect itself using the same strategy. In the face of massive hemorrhage, injured blood vessels spasm and shut themselves off to prevent further loss. Elsewhere, vessels in the extremities constrict, forcing blood back toward the central, vital organs, temporarily depriving less important tissues but returning more blood to the heart. This reflexive recoil of peripheral capillaries near the surface of the skin is partly what accounts for the pale appearance of trauma victims. But the body's response to trauma goes beyond the heart and its system of blood vessels.
Hormones pour into the bloodstream, mobilizing fuel stores from fat and raising the body's sugar levels. The protein in muscle, too, begins to be broken down and its constituent components recycled to assist in the defense, like a country putting its economy onto a war footing.
But the most complex and problematic aspect of the human body's response to major trauma is that of the immune system. At the site of injury, white blood cells patrolling in the bloodstream and the cells lining injured vessels and tissues release messenger molecules. These summon a host of other immune cells that take part in removing dead and damaged material and prepare the way for healing. In moderate injury, it is a beautifully orchestrated process that sweeps away cells that are no longer viable and replaces them with new ones, all the while making sure that enough energy is made available to cope with the increased metabolic demand of this restoration.
These mechanisms evolved over millions of years. They are what allowed our ancestors to hunt and to defend their familiesâto be predator and preyâand then limp off into the bushes and return rebuilt. For minor and moderate injuryâdeep lacerations and wounds that don't involve vital organs or uncontrolled blood lossâthe body's response has been carefully honed over Darwinian timescales to work in our favor, assisting our survival and ensuring that our genes continue.
But for severe injuries of the type that would have killed a person quickly in the days before modern medical intervention, no appropriate survival process has evolved. Instead the immune response to trauma oscillates wildly, causing more harm than good. The immune response is effectively like firing up a nuclear power station. You want to encourage the reaction to kick off, go critical, and generate heat, but you have to moderate it well enough to avoid meltdown. Underactivation would leave the victim prone to infection. Overactivation would lead to the malfunction of our organ systems, the biological equivalent of meltdown.
There is no evolutionary precedent for the limits of survival we are now probing. By the time we're supporting multiple organ systems on an intensive-care unit in the wake of major trauma, we've left evolution far behind. Out at those extremes, we depend not on our physiology but upon state-of-the-art systems of life support and the speed with which they can be brought to bear. The idea that, in the event of major accident, a team might literally drop out of the sky, scoop you up from the road, and propel you within minutes to a hospital is a construct of modern medicine that has existed only in recent decades. The edge of life, in that respect, has never been more heavily invested in. Expectations of survival in the face of horrific physical injury and physiological insult have never been so high. All of this means that today, when faced with even the most extreme trauma, we are less willing to accept defeat.
â
W
HEN THE BOMB SITE WAS CLEAR
of all the major casualties, we moved up to Soho Square to check over the walking wounded. We walked along Dean Street. The cafés and bars were entirely vacant, their tables covered with half-eaten meals and hurriedly left drinks. Afterward, we returned to the hospital, and I worked through the night.
The pub that had been bombed was called the Admiral Duncan. It was a bar popular with gay men. The bomber, a twenty-three-year-old paranoid schizophrenic and former member of the ultra-right British National Party, had planted and detonated two previous devices in the preceding fortnightâone in Brick Lane and one in Brixton. The bomb in Soho was the first one to inflict fatalities.
â
O
N
F
RIDAY,
A
PRIL 30, 1999,
A
NDREA
D
YKES
and her husband, Julian, traveled to London. John Light, who had been the best man at their wedding, was with them. Andrea was newly pregnant, and they were in a celebratory mood; John was to be godfather. They were on their way to the theater to watch the musical
Mamma Mia!
but decided to stop for a drink at the Admiral Duncan. They were joined by John's friend and former partner, Nick Moore.
The bomb detonated at 6:37
P.M.
More than a hundred people were injured. The blast killed Andrea and Nick instantly. John died the following day. The nine other casualties admitted to intensive care all ran difficult and prolonged courses, but all of them survived.
On June 30, 2000, David Copeland was found guilty of the murder of Nick Moore, Andrea Dykes, and John Light. In 2007 the High Court ruled that he must serve at least fifty years in prison.
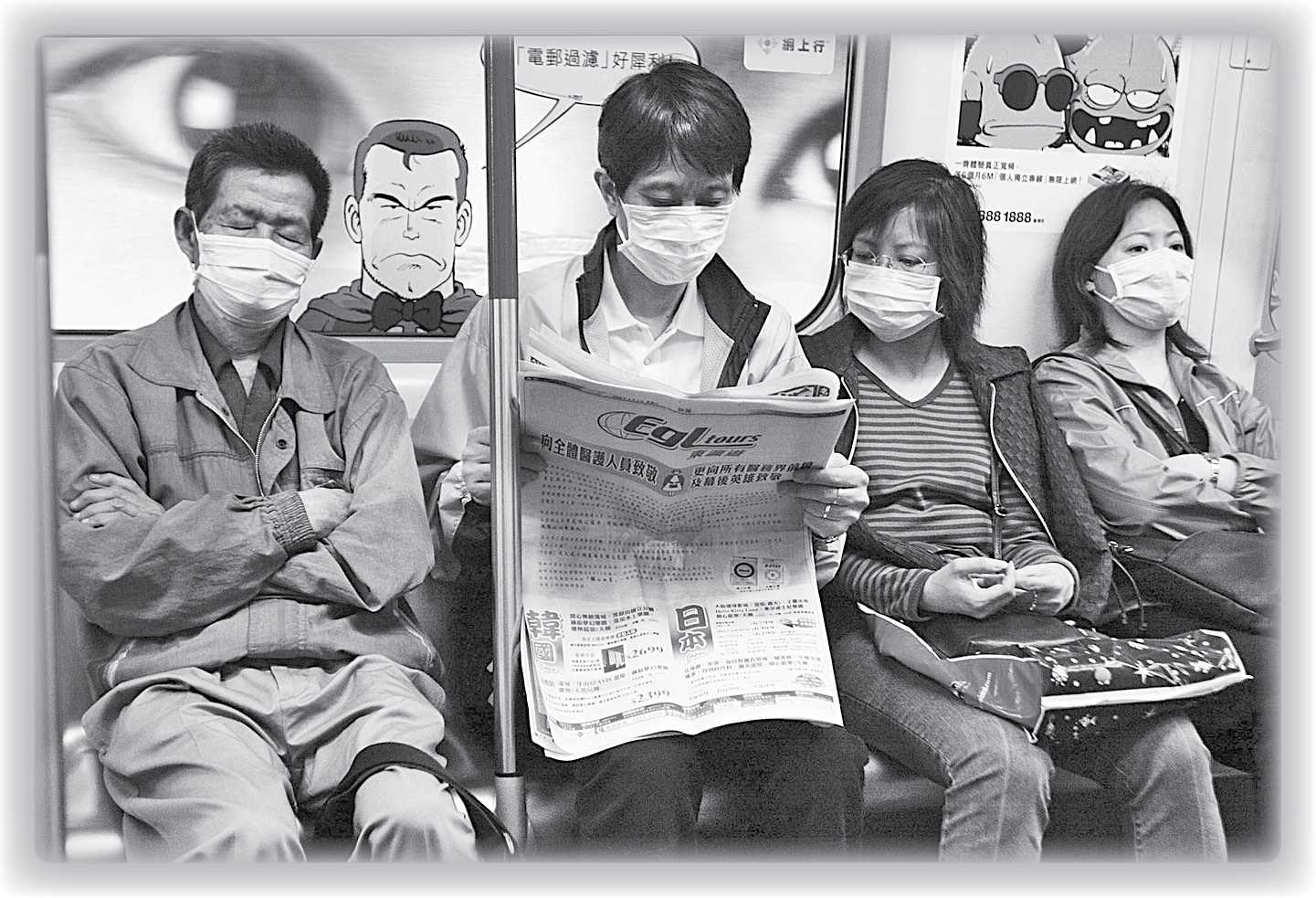
April 2003: Passengers on Hong Kong's Mass Transit Railway (MTR) during the severe acute respiratory syndrome (SARS) outbreak.
(© AFP/Getty Images)
T
he patterns on the electrocardiogram (ECG) screen trip over one another, degenerating once more from the essential electrical rhythm of life, becoming something more lethal. The patient is eighteen years old, and I don't know what's wrong. The nurses charge up the defibrillator again. We deliver the shock to try to escape this downward spiral. There is a pause. The cells of the heart reset themselves, and then a more normal rhythm returns.
We have taken blood, shot X-rays, and run CT scans in search of a diagnosis. There is little there to guide us. We have examined him from head to toe. His chest is clear, he is free from injury, and his kidneys appear to be workingâat least for now. But his blood chemistry is a mess. Lactic acidâa toxic by-product of the body's metabolismâis building up fast. Normally his kidneys and lungs would clear it from the circulation, but they are overwhelmed. Lying there in the bed, unconscious and ventilated, surrounded by the blinking lights of enough monitors to put a Christmas tree to shame, his heart driven by drugs, his lungs driven by a machine, he has the physiology of a man exhausted and on the verge of death. The ECG degenerates once more. We shock again.
His belly is slightly swollen. Perhaps there is a problem with his gut. Perhaps, somehow, a branch of the circulation that supplies the loops of bowel has become obstructed or compromised. That would be more than enough to make him critically unwell. But he's really too young for that to be likely. We review the CT scan images. To our eyes they are unremarkable. None of it adds up. We call in the surgeons. They are reluctant to operate. If they take him to surgery, he'll probably die on the table. But if we do nothing, he will die for sure. We debate the decision, and while we do so, I shock him again. It is perhaps the tenth defibrillation. I have lost count.
This is intensive care. We can support hearts, replace kidneys, ventilate lungs. We can resuscitate, render unconscious, and replenish. This is the sharp edge of all that can be done to support human physiology against illness and injury. This is everything we have, and still I cannot see how we can possibly win. When is enough enough? Perhaps the surgeons are right. It is, after all, absurdâextruding a man's physiology to its very limits in this way, well beyond any realistic expectation of survival. Why should we set ourselves against these catastrophes, when there are other fights that might be more easily won?
The formidable systems of artificial life support at modern medicine's disposal create new problems. The desire to find something more that we could do in the struggle to save life is sometimes replaced by the need to understand when to stop. To help understand why we try at allâand the events that gave birth to the first intensive-care unitsâwe must first go back to a time and place where modern medical interventions would have seemed like the stuff of science fiction and technology presented little obstacle to death.
â
T
HE VILLAGE OF
G
RAND
G
AUBE,
on the tiny island of Mauritius, is set back inland only a few hundred feet from the Indian Ocean. In 1946 it was a ramshackle collection of the most basic dwellings, separated from the sea by a beach of brilliant white sand. My father, Ah Yoong, and his family lived in a single-roomed hut. He was nine years old and shared the floor space with his parents, his two brothers, Daniel and John, and three sisters, Angele, Pierrette, and Therese. The roof was made of corrugated iron, and the walls were made of stone with barred openings that served as windows. It was, in my father's estimation, the best house in the village by far.
His parents, Li Moon Ki and Tang Tin Ying, were immigrants from China, finding their way from the southeastern Chinese province of Guangdong, via the oceangoing trade routes, to Mauritius. They were Hakka peopleâliterally “the visitors”ânomadic over centuries, moving where the land was good, never limited by geographical boundaries. When the age of steam came, they boarded ships in search of prosperity. That journey ended in Mauritius, a tiny volcanic island maybe thirty miles wide and not much more in length, fringed by white beaches and a vibrant coral reef. Tang Tin Ying was by all accounts a woman of fierce character and intelligence, but she was illiterate. Li Moon Ki, however, was among the few men of the village who could read and write. The house doubled as a general store, selling everything from rice and spices to liquor and nails.
Grand Gaube was a fishing village, a ramshackle assembly of huts with wooden walls, thatched roofs, and cow-dung floors. There were outside standpipes bringing fresh water, but only the most basic sanitation.
For the residents of Grand Gaube, the sea was their life. They took its spoils and were hostage to its temperament. They were vulnerable to the tropical storms it brought, particularly its cyclones. In the summer of 1945, two cyclones passed near Mauritius and a third descended on the island directly. These spiraling winds, with gusts of over a hundred miles an hour, carried drenching rains and destroyed what little infrastructure villages like Grand Gaube had. Afterward my father and his siblings collected the fish freshly strewn along the beach and swam in newly formed pools brought by storm and tides that had run inland. But sewage had spilled into these waters, and disease swiftly followed.
That summer an epidemic of polio broke out on Mauritius, causing as much devastation as the cyclones. The virus causing the disease could be carried in the gut and then spread in feces. Poor hygiene, the destruction of infrastructure, and bouts of diarrheal illnesses following the cyclone all conspired to amplify the spread. A team of British epidemiologists tracked it as it moved from village to village, often carried by healthy adults who'd built up an immunity to the virus.
What followed is an example of what happens when a transmissible, disabling, and potentially fatal disease encounters a population with only the most rudimentary public health provisions. During that summer, there were more than a thousand cases of poliomyelitis on the island. The children were by far the worst affected. Of 851 cases identified and recorded by epidemiologists, around two thirds were under the age of five, and more than 90 percent were under ten. The virus was aggressive and unfettered by modern medicine. Almost every case identified by the epidemiology teamsânineteen out of every twentyâsuffered paralysis and withering of one or more limbs.
In my father's family, his older sister, Angele, was the first to fall sick. For days she suffered with high fevers and drenching sweats. Grand Gaube had no doctor of its own. Occasionally a physician would pass through the village, but he was seen as a charlatan and viewed with distrust by most of its residents. Ah Yoong was sent out by his father to pick the leaves of the lilac tree, from which a cool bed could be made, insulating Angele from the hot floor in the hope that this would somehow reduce the fever. But the fever continued, and Angele appeared to be getting weaker.
In the earliest days of the illness, Ah Yoong would take his older sister by the arm to help her walk. Later he resorted to carrying her on his back.
Eventually the fever passed, but Angele was left paralyzed, unable to walk. She was just nine years old.
â
T
HE BASIS FOR THE CONSCIOUS PROCESS
that triggers us to move a limb, speak a word, or register a thought remains elusive and likely will for some time to come. Consciousness is the last dark continent of life science. We are incapable of properly defining it, much less understanding how it works.
But the processes it sets in motion are better understood. When it comes to movement, we know that the motor cortex is the point of origin of signals that trigger voluntary movement.
You can get an idea of the location of this thin strip of brain by putting your thumb on your earlobe and then stretching your index finger up until it reaches the top of your skull. Below the quarter arc now made by your finger and thumb, beneath the layers of skin, bone, and tough protective tissues, lies a narrow strip of brain. It is less than a centimeter wide and penetrates to only a few millimeters below the brain's surface. In this modest layer lies a population of pyramid-shaped cells from which the impulses that initiate movement are first fired. Those nerve cells are neurons, responsible for connecting thought to action, specialized for the task of transmitting signals from brain to muscle bed.
Most of us could have a good crack at drawing an animal cell. You'd start with an indefinite oval, and somewhere near its center, you'd plant a circle that you would shade in and call the nucleus. A couple of smaller scribbles around that nucleus would give you mitochondria, ribosomes, Golgi apparatus, and other organelles. But this is only the basic scheme. Not all cells are made equal. And when it comes to neurons, that sketch doesn't quite cover it.
The word
cell
derives from
cellula,
the Latin word for a room. But the whole thing is built much more like a walled city. The important stuffâthe executive decision makingâis done in the nucleus, the town hall. Here densely packed double-stranded DNA is woven and storedâthe blueprints from which your body, and indeed all life, is built. The surrounding clear cytoplasm is dotted with tiny organelles, much smaller than the nucleus, which function like a city's utilities and amenities. Here the mitochondria serve as power stations, while ribosomes are industrial estates, given over to the execution of manufacturing orders handed down from the nucleus. Elsewhere in the cytoplasm, there are other microscopic structures that play structural roles or take part in waste disposal or defense.
The pyramidal nerve cells of the brain's motor cortex stretch out over vast distances within the body. The extensions of the cell are called axons. For the longest neurons in the body, those axons can grow to be over a meter in lengthâan enormous distance, given the minute scale of the cell itself. To put that into context, consider this: If the cell body of the motor neutron were indeed a city, say about the size of London, its axon would be represented by a road that ran out into space for about twenty million miles (which would get you about halfway to Mars!)
The neuron sends its axon down through the brain, on into the brain stem, and through the spinal cord, running and converging with others, like individual telephone wires combining to form the main trunk. Most of them eventually cross over to the other side of the body (which is why a stroke on the left side of the brain can lead to paralysis on the right side of the body). In the front of the spinal cord, they end. This nerve cell, the first link in the path from brain to muscle, is called the upper motor neuron. It has so far carried a nerve impulse from the brain to what is essentially a junction box in the spinal cord.
Here in a location known as the anterior horn, it will form a synapse, connecting with a final neuron, completing the link between the events in the brain that provide the impulse to move and the physical means by which movement is achieved: the contraction of muscle. This second nerve cell, the lower motor neuron, runs from the spinal cord, and its axon finishes embedded in the substance of a skeletal muscle.
It is the junction of these two neurons in the anterior horn that is vulnerable to attack by the polio virus. If it invades and destroys the cell body of the neuron, then the entire cellular structure, from spinal cord to muscle, dies back tooâfor good.
The cells of the nervous system are the oldest in your body. In contrast to almost every other cell type in the human body, they lack the ability to divide and self-replicate. Unlike skin cells, which enjoy a hefty turnover, if neurons become irretrievably damaged or die, they are not replaced.
To partially compensate for this lack of ability to regenerate, the central nervous system is buried deep within the core of the body, encased within the column of bone that is your spine and protected in the vault of your skull.
Despite this, it remains vulnerable, especially in the face of modern threats like motor transport. And the armor of the skeleton is no protection against infection.
During an attack of poliomyelitis, many thousands of these lower motor neurons can be lost. Once deprived of their nerve supply, the muscles supplied begin to waste, giving the characteristic appearance of withered limbs that accompanies paralytic polio.
â
W
HEN YOU TALK TO VIROLOGISTS
about viruses, they have a grudging respect for their foe. Incapable of independent existence, viruses rely upon entering more complex cells and hijacking both their metabolic and reproductive machinery. Their genomes are too restricted in information content to allow them to manufacture the means of their own survival. They have only the simplest instruction setâone that allows them to attach to and enter a cell and trick it into manufacturing further copies of the virus.
But these simple structures have the capacity to destroy the host cells they invade and then spread like wildfireâfirst from cell to cell and then from person to person. As a consequence, viral pandemics are capable of causing death, disease, and personal suffering in many millions.
By the time the epidemic in Mauritius had passed, my father's older sister, Angele, was wheelchair bound. His younger sister, Therese, was less fortunate still. In her the polio virus had weakened the muscles responsible for breathing and those involved in swallowing. She went on to die of pneumonia.
â
I
N 1952 THE POLIO VIRUS ARRIVED
in northern Europe. But the pattern of attack was very different from that seen in Mauritius. Poliomyelitis, the inflammation and destruction of the motor nerves brought about by the polio virus, is also known as infantile paralysis because in earlier epidemics it was almost invariably young children who were most severely affected.
That pattern of attack and disability continued in developing countries like Mauritius, but in Europe polio had for some time been confined to small outbreaks because of improved sanitation, so there was little in the way of natural immunity to the virus among the wider community. When the epidemic arrived in Copenhagen in the summer of 1952, the disease ran rife in adults and children alike. The manifestation of the disease in adults was far more severe with a much higher risk of paralysis of the muscles involved in breathing and swallowing. This form of the diseaseâhitherto rarely seen in polio epidemicsâwas commonly fatal.
