Resident Readiness General Surgery (54 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

An initial failure to void after anesthesia is likely a drug effect. A second or third failure should raise suspicion for obstructive or neurogenic pathology, especially in patients with additional risk factors.
COMPREHENSION QUESTIONS
1.
Which of these patients is at highest risk of developing POUR?
A. A 40-year-old hypertensive male undergoing systemic analgesia for wide local excision of a forearm melanoma.
B. A 22-year-old female who is 10 weeks pregnant undergoing general anesthesia for a laparoscopic appendectomy.
C. A 70-year-old female with well-controlled diabetes undergoing spinal anesthesia for left greater saphenous vein radio-frequency ablation and stab phlebectomy.
D. A 65-year-old male with BPH undergoing general anesthesia with epidural analgesia for a laparoscopic right inguinal hernia repair.
2.
Which of the following is true?
A. The first step in evaluation of POUR is to obtain an intermittent catheterization.
B. In a patient with POUR who has a known urethral stricture and hematuria after initial intermittent catheterization, it is appropriate to proceed with intermittent catheterizations until physiologic micturition normalizes.
C. After obtaining a bladder scan with 400 cm
3
intravesicular volume 6 hours postoperatively, a single intermittent catheterization is the appropriate first step.
D. A volume of 1000 cm
3
urine output on intermittent catheterization is unlikely to cause detrusor dysfunction in a patient with no prior history of urinary obstruction.
3.
Which of the following is most sensitive and specific for determining the initial presence of POUR?
A. Patient complaint of low abdominal pain and failure to void
B. Clinical examination of a palpable bladder with dullness to the umbilicus
C. Bladder ultrasound
D. Bladder catheterization
Answers
1.
D
. This patient has obstructive pathology, is advanced in age, is male, and is receiving general anesthesia for a procedure with a high risk of urinary retention.
2.
C
. Parasympathetics trigger detrusor contractions and relax the internal urethral sphincter. Sympathetics relax the detrusor and tighten the internal urethral sphincter. In the immediate postoperative period there is excess sympathetic tone. A little extra time can be all that is required for that balance to normalize and allow the patient to recover the ability to urinate. In other words, don’t rush to place a catheter for a problem that may resolve on its own in another few hours.
3.
C
. Bladder ultrasound is noninvasive and can provide an estimated volume of urine being retained to guide further management choices.
 A 52-year-old Female Who Is Dehydrated Postoperative Day #1
A 52-year-old Female Who Is Dehydrated Postoperative Day #1
Aisha Shaheen, MD, MHA and Marie Crandall, MD, MPH
During your morning pre-rounds you see Ms. Yang, a 52-year-old female who is POD #1 from a small bowel resection for a high-grade obstruction. Ms. Yang states her pain is well controlled with medication but she feels tired and a little light-headed. In checking her postoperative orders you note she is NPO, her naso-gastric tube should be attached to continuous wall suction, and she should have IV fluids running. Although the NGT is in place and appears to be functioning properly, you notice on closer inspection her IV fluid tubing is disconnected. The patient tells you the tubing was bothering her while she was sleeping, so she disconnected it during the night. Her vitals reveal her to be mildly tachycardic and hypotensive with a heart rate of 103 and a blood pressure of 98/70. As you examine her, you notice her mouth and lips are dry and she is clearly dehydrated.
Her wound dressings are clean, dry, and intact, and her exam is otherwise unremarkable. You realize the patient needs to be given fluids.
1.
What type of intravenous fluid is most like plasma?
2.
For each of the following types of fluid loss, what type of crystalloid solution is most appropriate and why?
A. Gastric losses
B. Pancreatic/biliary/small bowel losses
C. Large intestine (diarrheal) losses
3.
What effect do crystalloids have compared with colloids on plasma volume expansion? On mortality?
4.
Estimate the patient in this vignette’s maintenance fluid requirement. Assume she weighs 80 kg. Now adjust this estimate based on a 24-hour NGT output loss of 600 cm
3
.
5.
If another patient, Ms. Bradford, was a cardiac patient with an ejection fraction of 31%, what precautions would need to be taken in administration of her maintenance fluid?
6.
If Ms. Bradford was diabetic, should her maintenance fluid contain dextrose?
IV FLUIDS
Answers
1.
Table 42-1
summarizes the ion concentrations in the 2 most common types of crystalloid fluids—normal saline (NS) and lactated Ringer’s (LR). Note that the
composition of LR most closely approximates that of plasma and is commonly used for surgical patients. However, because of the addition of calcium and lactate (bicarbonate) to this solution, it should not be used in certain clinical scenarios. For example, the calcium in LR can bind to certain drugs including amphotericin, ampicillin, and thiopental and reduce their effectiveness. Preclinical studies have also shown that calcium can bind to the anticoagulant in donor blood and promote clot formation; therefore, in clinical practice many centers do not infuse LR simultaneously with red blood cell transfusions.
Table 42-1.
The Concentration of Ions in Common Crystalloid Fluids Compared With Plasma
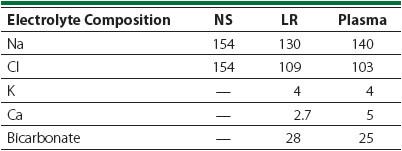
There are no clear contraindications to the use of NS. However, it is important to know that the high chloride concentration of this solution can lead to a non-anion gap (hyperchloremic) metabolic acidosis if large volumes are infused.
Understanding the tonicity of various crystalloid fluids is important when deciding what to use for resuscitation and for maintenance. Both NS and LR are isotonic fluids, meaning the osmolar concentration of these solutions is the same as that of the interstitial space. Infusion of isotonic fluids into the vascular space results in diffusion of the fluid until it is evenly distributed among all of the fluid compartments of the body. About 1/3 of the total volume of infused isotonic crystalloid stays within the vessels. Isotonic solutions can be used for resuscitation or for maintenance. Hypotonic solutions (eg, 0.45% NS), in contrast, have a lower osmolar concentration than the intracellular and interstitial space. As a result, more of the water leaves the intravascular space in order to achieve osmolar equilibration with the interstitium. Because the water in hypotonic crystalloid leaves the intravascular space more rapidly than isotonic solutions, hypotonic solutions are never used for resuscitation. They are commonly used for maintenance fluid administration, as the insensible losses they are meant to replace are typically hypotonic in nature (ie, more water is lost than solutes).
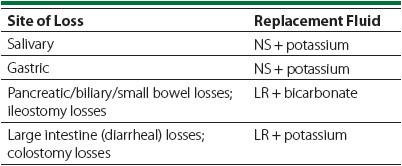
2.
The most appropriate crystalloid to use for losses from the gastrointestinal tract depends on the area of the loss—each portion of the GI tract has a different electrolyte composition. Replacement should be chosen to match, as closely as possible, the composition of those losses (see
Table 42-2
).
Table 42-2.
Fluid Losses and Recommended Replacements
3.
Crystalloid fluids are those fluids that contain only water and dissolved salts. Colloids are fluids that contain water and larger molecules or even cells (eg, albumin, packed red blood cells). Crystalloid fluid contains only small molecules, and they distribute freely throughout the extravascular space. As discussed above, when crystalloid fluids are administered, the interstitial volume expands more than the intravascular plasma volume. In contrast, the large molecules and/or cells in colloid fluids do not diffuse readily between body fluid spaces and remain intravascular. This creates an osmotic pressure that attracts water and thereby preferentially expands the intravascular plasma volume. For this reason, conventional teaching suggests 3 L of crystalloid solution is required to obtain the same incremental increase to plasma volume obtained with just 1 L of colloid solution. For those situations in which a patient cannot tolerate large volumes of fluid, colloids (albumin in particular) are widely used.
While the theoretical basis for this practice may be sound, there are no clinical trials that have demonstrated any difference in outcomes when using crystalloid or the most commonly used colloid, albumin. For example, the Saline versus Albumin Fluid Evaluation (SAFE) study showed that the type of fluid administered (colloid vs crystalloid) conferred no survival benefit in critically ill patients. The uncertain evidence combined with the significantly higher costs of colloid solutions suggests that crystalloid solutions should continue to be preferred over albumin for most routine clinical situations.
