Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (222 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

2. Beta-HCG level: It should be obtained to exclude pregnancy.
3. Serum TSH: For the evaluation of hyper- or hypothyroidism.
4. Consider a workup for less common endocrinopathies such as Cushing syndrome and acromegaly after excluding more common causes and only if history and physical findings raise clinical suspicion.
Imaging Studies
High-resolution CT scan or MRI is useful for localization of pituitary tumors.
Suggested Readings
Golshan M, Iglehart D. Nipple discharge. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Snyder PJ. Causes of hyperprolactinemia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Snyder PJ. Clinical manifestations and diagnosis of hyperprolactinemia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
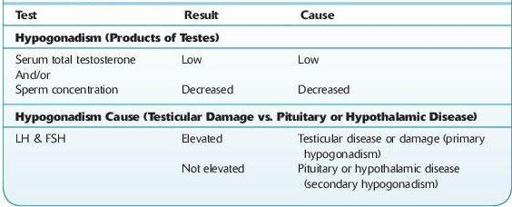
MALE HYPOGONADISM* (Table
6-7
)
Definition
Male hypogonadism refers to decrease in one or both testicular functions—sperm production and/or testosterone production. The root cause is either a disease of or damage to the testes (primary hypogonadism) or a disease of the pituitary or hypothalamus (secondary hypogonadism).
Table 6-7 Laboratory Diagnosis of Male Hypogonadism and Primary versus Secondary Causes
*Submitted by Charles R. Kiefer, PhD.
Who Should be Suspected?
In general, early manifestations in postpubertal males include decreased energy and libido, whereas later manifestations include decreased androgen-dependent development of hair, muscle mass, and bone mineral density. However, there are age-related or physiologic considerations.
Manifestations in infants may include ambiguous genitalia or cryptorchidism (bearing in mind that a retractile testis usually descends into the scrotum within the first year of life). A micropenis at birth may indicate deficient gonadotropin-releasing hormone during the third trimester of pregnancy.
Manifestations in teenage boys may be signaled by failure to develop pubertal changes at the normal rate, resulting from low serum testosterone and normal or subnormal concentrations of LH (luteinizing hormone) and/or FSH (follicle stimulating hormone). If just delayed puberty, it will correct spontaneously. However, it may be the result of secondary hypogonadism, which becomes a more likely possibility the longer the delay.
In the severely obese (BMI > 40), there may be secondary hypogonadism as well as decreasing the serum concentration of sex hormone–binding protein.
In older men undergoing male senescence, although serum total testosterone falls slightly, free testosterone falls more significantly, so that levels after age 80 are one half to one third of those at age 20.
Within each of the two classes of male hypogonadism (primary or secondary), there exist both congenital and acquired causes. Primary congenital causes include Klinefelter syndrome (47XXY) and androgen synthesis disorders; whereas primary acquired causes include infection (e.g., mumps, orchitis), trauma, and chemotherapy or radiation therapy. Secondary congenital causes include Kallmann syndrome, hypopituitarism, and idiopathic hypogonadotropic hypogonadism; whereas secondary acquired causes include mass lesions in the pituitary or hypothalamus, hyperprolactinemia, and trauma to the base of the skull.
Laboratory Findings
The salient diagnostic test for male hypogonadism is measurement of serum testosterone concentration—a low value being indicative of the condition. Serum total testosterone (free plus protein bound) accurately reflects secretion of testosterone in most cases. Measurement of free testosterone concentration could be considered in cases of obesity (reduces testosterone protein binding) or male senescence (slightly increases protein binding). Time of serum collection from young men should take into account diurnal variation of testosterone levels, which are maximal at about 8 AM and minimal at about 8 pM (about 70% of maximum). Measurement should be repeated if the first 8 am value is low or borderline, or at variance with the clinical picture. If testosterone levels are normal, and infertility is a problem, then a semen analysis should be obtained for further workup.
