The Lupus Book: A Guide for Patients and Their Families, Third Edition (33 page)
Read The Lupus Book: A Guide for Patients and Their Families, Third Edition Online
Authors: Daniel J. Wallace

mouse bite on x-rays. Lupus induces joint deformities less than 10 percent of
the time and erosions are almost never seen. An occasional patient has distinct features that fulfill the ACR criteria for both RA and SLE. Called
rhupus
, this rare disorder is managed with drugs useful for both diseases, such as nonsteroidals, steroids, methotrexate, and antimalarials.
Most patients with
scleroderma
, an autoimmune disease characterized by inflammation that heals with tightening of the skin and scarring of the tissues,
also have a positive ANA. The 200,000 Americans with scleroderma-related
disorders (e.g., progressive systemic sclerosis, CREST syndrome—or
Calcino-
sis, Raynaud’s, Esophagitis, Sclerodactyly, Telangiectasia
—autoimmune Raynaud’s, mixed connective tissue disease) are frequently misdiagnosed as having
SLE. A few lupus patients fulfill criteria for both diseases (called
lupoderma
), and in most cases the condition eventually evolves into a pure scleroderma. In
reality, a process known as
mixed connective tissue disease
(
MCTD
) probably makes up the majority of these cases. By definition, as well as being ANA-positive, MCTD patients must have a positive anti-RNP. Their condition resem-
bles lupus, but they tend to have puffy hands, complain of heartburn and swal-
lowing problems, are at an increased risk for developing pulmonary hypertension and have interstitial scarring of the lungs on chest x-ray. Raynaud’s phenomenon is almost universally seen in MCTD. Our survey of 464 patients with SLE shows
that 25, or 5 percent, also met the definition for MCTD.
Inflammatory myositis
, as in dermatomyositis or polymyositis, is a feature of lupus in 10 to 15 percent of patients. However, the very high CPKs seen in
Is It Really Lupus?
[175]
dermato- or polymyositis, its distinct skin papules, and its association with malignancy and helioptrope-like rashes are not observed in SLE. In other words,
lupus is occasionally characterized by a mild, bland, frequently asymptomatic
muscle inflammatory process.
Rheumatoid arthritis, lupus, scleroderma, inflammatory myositis, and MCTD
all involve inflammation of the small and medium-sized arteries and arterioles.
Polyarteritis nodosa
and
microscopic polyangiitis
are primary vasculitides of those caliber vessels. They can mimic lupus and most patients have a positive
ANA. The diagnosis of polyarteritis or microscopic polyangiitis is confirmed by blood testing (known as ANCA, or antinuclear cytoplasmic antigens) fairly specific for systemic vasculitis, along with evidence of inflammation of the vessels documented by an angiogram or biopsy. A group of patients have features of
two to six of the disorders mentioned above, but do not seem to fit perfectly
into any one of them. They are said to have a
crossover syndrome
. Many individuals initially exhibit a crossover syndrome that evolves into a distinct, de-finable disorder over time. Occasionally, rare forms of vasculitis affect medium and small-sized vessels, which heal with scars known as granulomas; these are
difficult to differentiate from lupus at first.
Wegener’s granulomatosis
and
Churg-Strauss granulomatous vasculitis
are ultimately diagnosed by the pathologic finding of granulomas or a positive c-ANCA blood test in Wegener’s.
An unusual form of vasculitis called
Behcet’s
is rarely diagnosed as ANA-negative lupus. Its features of mouth ulcers, eye inflammation, and central nervous system involvement resemble SLE, but the lack of a positive ANA usually
leads physicians to a correct diagnosis. Finally, as mentioned in the last chapter, older people can develop an aching in the hips and shoulders with severe stiffness and a high sedimentation rate. Some of these individuals, who are ulti-
mately diagnosed with
polymyalgia rheumatica
, have positive ANAs as a function of age, and lupus must be ruled out.
Several features of autoimmune disease can also appear by themselves without
fulfilling criteria for any of the disorders above mentioned. These include Raynaud’s phenomenon, idiopathic thrombocytopenic purpura (ITP), and Sjo¨gren’s
syndrome, in addition to those listed in the above paragraph.
DOES LUPUS DECREASE THE RISK
OF GETTING OTHER DISEASES?
For reasons that are not clear, several disorders have a ‘‘negative’’ association with lupus—in other words, having lupus decreases your chances of getting
certain diseases. These include
amyloidosis, sarcoidosis, ankylosing spondylitis
, and HIV infection.
Since 500,000 to 1 million Americans had SLE and at least 50,000 of them
received blood transfusions between 1978 and 1983 when our blood supply was
[176]
Where and How Can the Body Be Affected by Lupus?
not safe, one would have expected some of the recipients to develop
AIDS
, a disease caused by the
human immunodeficiency virus
. In fact, not a single case was reported. (The 50,000 figure is derived from adding the number of lupus
patients on dialysis who would have been given frequent transfusions, the num-
ber of orthopedic surgeries such as hip replacements for avascular necrosis,
lupus patients with autoimmune hemolytic anemia, and the common use of
transfusions over a 5-year period in that era for gynecologic surgery. With the advent of the drug EPO, we rarely give transfusions to patients on dialysis, and patients can now donate their own blood prior to surgery.)
Even though 90 percent of AIDS patients in the United States are males and
90 percent with SLE are female, statistically one would still expect numerous
cases of AIDS with SLE. However, at the time of this writing, only fewer than
100 have been reported in the world’s literature. Some were children with con-
genital AIDS who developed SLE, and others received a kidney transplant from
a human immunodeficiency virus (HIV)-positive donor. Only a few adults had
both disorders.
Does lupus protect patients from AIDS? Since they represent opposite poles
of the immune system (AIDS patients have few CD4 cells and lupus patients
have overactive CD4 cells), this possibility is an intriguing one which deserves further study. Interestingly, I have occasionally come across lupus patients with false-positive HIV tests; this phenomenon may reflect the ability of SLE to
produce antibodies to many different viruses. Nevertheless, lupus patients must be cautioned not to let their guard down, to practice safe sex, and to avoid street drugs.
WHAT IS THE RELATIONSHIP BETWEEN
LUPUS AND FIBROMYALGIA?
Fibromyalgia, or fibrositis, has repeatedly been mentioned throughout this book.
Here’s where you find out just what it is.
What Is Fibromyalgia?
Fibromyalgia is a syndrome that afflicts 6 million Americans. About 90 percent
of them are women, and most develop it between the ages of 20 and 50. It is
a pain-amplification syndrome characterized by chronic neuromuscular pain,
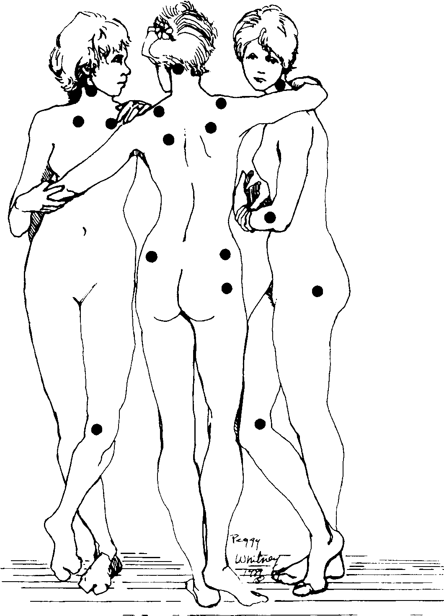
widespread stiffness and aching of at least 3 months duration. In order to fulfill the ACR criteria for fibromyalgia, one must have tender points (defined as winc-ing or withdrawing in pain when 4 kilograms or 9 pounds of pressure is applied) in at least 11 of 18 designated points in all four quadrants of the body (right side, left side, above the waist, and below the waist, as shown in Figure 23.1).
If tender points are found in fewer than four quadrants, the patient does not
Is It Really Lupus?
[177]
Fig. 23.1.
Tender Point Locations in Fibromyalgia
have fibromyalgia but a
regional myofascial syndrome
. Most of the tender points are in the upper back and neck area, buttocks, and chest. In addition to musculoskeletal symptoms, patients with fibromyalgia may complain of nonresto-
rative sleep (waking up in the morning after lying down for 8 hours but not
feeling refreshed); functional bowel symptoms such as abdominal cramping,
bloating, and distension; a sensation of swelling with numbness and tingling;
profound fatigue; and occasionally cognitive dysfunction. These symptoms are
similar to those discussed in Chapter 15.
The cause of fibromyalgia is unknown, but pain amplification probably results
from a dysfunctional interaction of neurotransmitters (such as epinephrine, do-
[178]
Where and How Can the Body Be Affected by Lupus?
pamine, or serotonin), the autonomic nervous system, hormones, and cytokines
(Chapter 5) when exposed to repetitive noxious stimuli. Fibromyalgia can be
brought on by trauma, infection, or an inflammatory disorder, among other
causes and is aggravted by psychosocial stressors.
How Many Lupus Patients Have Fibromyalgia?
Several surveys have suggested that about 20 percent of all lupus patients also fulfill the ACR criteria for fibromyalgia. The most common causes of fibromyalgia in SLE are a reaction to active musculoskeletal lupus, transient symp-
toms after a viral infection or trauma, poor coping mechanisms, and a steroid
withdrawal syndrome. The latter occurs, for example, when your doctor sees
how well things are going and decreases prednisone doses from 20 to 15 mil-
ligrams a day. Decreased steroid doses can result in a flareup of muscle and
joint aching without a worsening in laboratory testing, objective synovitis, or swelling indicating a lupus flare. These symptoms often lead patients to call
their doctors, who then raise the prednisone back to 20 milligrams daily. This
may be a mistake. These complaints represent withdrawal symptoms and will
disappear spontaneously over a 1- to 3-week period. Not only do alterations in
steroid doses aggravate fibromyalgia, but the skin of all patients on corticosteroids develops an increased sensitivity to pressure which imitates fibrositis.
How Can We Tell Lupus from Fibromyalgia?
Differentiating active lupus from fibromyalgia is critical. This is often made
difficult by two confounding factors: lupus patients can have concurrent fibro-
myalgia, and 10 percent of fibromyalgia patients have a positive ANA. In pa-
tients with SLE, complaints of fatigue, muscle aching, and stiffness can represent active lupus or fibrositis. If a recent infection, trauma, adrenal insufficiency or steroid tapering is ruled out, active lupus is usually detected by the presence of a rash or swollen joints on physical examination or is evident in tests for anemia, elevated sedimentation rate, a high anti-DNA, or low complement levels. A
common mistake among internists and even rheumatologists is to take a patient’s symptoms at face value and treat them with toxic medication even though no
laboratory parameter validates that a lupus flareup is present. Fibromyalgia flareups respond only temporarily to rises in corticosteroids, and the patient may
actually feel worse within several weeks.
How Do Doctors Treat Fibromyalgia?
Fibromyalgia is managed in several ways. First, doctors reassure patients that
even though it’s a real disease, it is neither life-threatening nor crippling. Rheumatologists usually provide brochures from the Arthritis Foundation or the
American Fibromyalgia Syndrome Association that document its nonprogressive
Is It Really Lupus?
[179]
nature. Second, physicians encourage patients with fibromyalgia to adjust their life-styles in a way that will ensure restful sleep, pacing of time, and improved coping mechanisms. Counseling may be recommended. Also, physical measures
such as moist heat, gentle massage, biofeedback, and coolant sprays followed
by muscle stretching (called spray and stretch) are also employed. An occasional injection of a local anesthetic (with or without a local steroid) can be used at the trigger point of pain. A patient’s work station and job description are analyzed in an effort to minimize alterations in body mechanics that could irritate muscles and stress joints. Electronic acupuncture (e.g., acuscope, neuroprobe,
TENS units) may also be helpful.
Finally, numerous medications can be tried. They include NSAIDs, which are
modestly helpful. Muscle relaxants such as Norgesic, Parafon, and Soma are
beneficial for a few hours. Tricyclic antidepressants—such as cyclobenzaprine
(Flexeril), doxepin (Sinequan), amitriptyline (Elavil), and nortriptyline (Pamelor)—promote restful sleep, relax muscles, minimize reactive depression, and
raise pain thresholds. Benzodiazepines such as diazepam (Valium), clonazepam
(Klonopin), and chlordiazepoxide (Librium) do the same thing but are poten-
