Surviving the Medical Meltdown (32 page)
Read Surviving the Medical Meltdown Online
Authors: Lee Hieb

Step 1: If footwear is removed or when the ankle is exposed, place padding above and around the boney prominences on each side of the ankle.

Step 2: Fold a 36-inch SAM Splint to create two equal halves.

Step 3: Apply C curves two-thirds of the distance down each half. Add reverse C curves on the edges if needed for strength. Do not extend the curves further or they will stiffen the splint and limit your ability to fold it around the foot or ankle.

Step 4: Fold the stirrup splint around the foot and ankle.
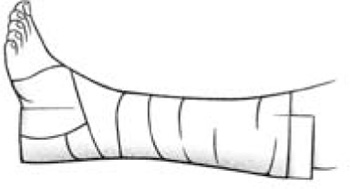
Step 5: Secure with your wrap of choice.
In concluding this chapter, as an orthopaedic surgeon, I cannot resist recounting a little history.
“Bone setting” is an ancient practice described in the oldest extant medical text – the Edwin Smith papyrus from Egypt, dated around 1500 BC. Although straightening and splinting fractures and dislocations uses very commonsense principles, the actual techniques have always required dexterity, experience, and skill. “Bonesetters” have always been a bit separate from the rest of medicine. Sometimes fracture care was done by barber-surgeons, but it was never practiced by “true” physicians. Friendly rivalry between internal medicine physicians and orthopaedists still exists. In primitive cultures the local witch doctor may have set bones, or he subcontracted to a specialist who did nothing but bone setting. Today, in spite of the spread of Western medicine generally, this practice continues in sub-Saharan Africa, where (as in Nigeria) nearly 85 percent of fracture care is rendered by traditional unlicensed “bonesetters.”
23
BACK AND NECK PAIN
I
keep a copy of a Gahan Wilson cartoon framed on my wall. In it, a patient is sitting on an examination table with his shirt off, and there is an ugly green lizard-like beast clinging to the patient’s back. The doctor, poking at the beastie with his finger, says, “Mr. Jones, I believe we’ve found the source of your back pain.” Although the cartoon is humorous, it brings up an important point: thorough clinical examination is a key component of diagnostic medicine. In today’s world of government-run health care, lesser-trained medical providers are replacing doctors, and all of us are being overwhelmed with computer work that takes time away from patient care. Careful physical examination is often skipped over. Many patients tell me, a spinal surgeon, that after going from doctor to doctor, I am the first one to actually have them undress and examine the back. But that is important because not all back pain is caused by spinal injury. I haven’t found a green lizard, but I have found a number of shingles rashes, and shingles will cause several weeks of back pain before it resolves. I have also found burns from heating pads, wallets that are too big to sit on repeatedly without compressing the sciatic nerve, and marks from too-heavy backpacks or overweighted police duty belts.
So all back pain is not from the spine. If your back pain is associated with vomiting, illness, alteration of bowel habits, and so forth, seek medical help. This chapter is for treatment of the everyday, garden-variety back pain.
Back pain is commonly due to an insult to the little joints in our spines or our disks – the hydraulic shock absorbers that separate the spinal bones. It is a popular misconception that back pain is muscular. Usually it is not. Muscle spasm is a secondary phenomenon caused by joint irritation.
The usual story goes something like this: “I was helping move furniture [or other objects] over a period of several hours. My back didn’t hurt right away, but later that night I started to have low back pain. By morning I could barely move. Any motion hurts, but its better when I lie down.”
This is the classic “overuse” syndrome. The little joints in the back get abused, so they swell and hurt. Usually this kind of back pain is better but not totally gone in three days. Treatment consists of rest; anti-inflammatories, such as Naproxen (440–500 mg, twice a day); a hot pack or ice to the area (whichever feels better); and time to resolve. You can stretch the lower back by lying on the floor with your legs over a chair or the couch seat and then bringing your knees slowly to your chest. Hold for ten seconds; then return to the starting position. Relax for thirty seconds, and then repeat the exercise a few times. Take the Naproxen every day until several days
after
you stop having pain, to prevent recurrence.
Disk injury:
A disk injury may start off just as the back pain did in the hypothetical furniture-moving case. Or it may occur with a sudden lifting, twisting injury, or with very little trauma at all. These disk problems usually occur in people over thirty who have done “daily microtrauma” to their disks by repeated bending, causing small cracks to occur in the outside elastic ring of the disk. These cracks eventually form a channel. Through this channel of cracks, the inside jelly part of the disk “herniates” into the outside of the disk,
giving you horrible back pain that can last for two to three weeks. Sometimes, the interior jelly material pushes
completely
outside of the disk, lodging next to the nerve that goes down your buttock and leg. This can give you the classic symptoms of
sciatica
– buttock and/or leg pain, burning, numbness, and worsening of pain with sitting or bending. You may also have some foot weakness. The treatment for disk damage is initially the same as for other back pain – rest, Naproxen, and time. This will take longer, usually two to three weeks. And total healing of the disk occurs over two years. To allow the channel to seal over and heal, it is important not to pressurize the disk by sitting, lifting, or forward bending. In general your activities at first should be limited to walking and standing or lying down. For at least two weeks, avoid sitting or bending. Take the Naproxen faithfully until the pain is gone for at least a week or two. If at any time you have progressive weakness, any inability to void, numbness in the groin area, loss of erectile function, or bowel incontinence – seek emergency help.
Of note, smoking is a leading cause of disk disease because one cigarette closes down the blood supply to the disk by 50 percent for twelve hours. So, your disks do not have the ability to heal themselves between episodes of use. To keep your back healthy, don’t smoke, stay thin, avoid repeated bending, and keep your core muscles in good shape.
Neck pain:
The principles for avoiding and treating back pain are generally true for neck pain too. Most neck pain is due to a lifetime of repeatedly looking down, flexing our necks. We were designed to be hunter-gatherers, spending most of our days looking out over the plains in search of game. Our heads were balanced on our torsos, and the little “rocker bearing” joints didn’t get overused. But today our civilized selves spend hours a day looking down at schoolbooks (or at a surgical patient), or we sit reading in bed with our necks too flexed. If you have neck pain, do as I recommended for the back. Rest the neck in a neutral, non-flexed position, take
Naproxen, and give it time. If arm pain or weakness develops and is progressive, seek help.
To prevent problems with your neck, avoid a prolonged flexed position. Don’t sleep on too big a pillow. Your neck and head need to be straight with the torso. Use a small, squishy, down pillow or a rolled-up towel. (The towel is helpful in avoiding neck pain in hotel rooms from those too-big, pretty pillows.) Don’t read without elevating your book. Dittos for knitting or other activities you might do in your bed. Put a pillow under your arms and raise up your work. On an airplane put that pillow under your lower back, not your head. Practice good posture, keeping your head balanced, like a ballerina, over your body.

good posture at a desk

bad posture at a desk

