Pediatric Examination and Board Review (78 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(D) endoscopic banding
(E) all of the above
ANSWERS
1.
(B)
Patients with evidence of hemodynamic compromise (HR 165 in a 4-year-old) must be stabilized before any workup.
2.
(B)
Fluid resuscitation should be the first step. Gastric lavage is not necessary. The description of the bleeding is from the lower GI tract. Although a vigorous upper GI bleed could cause passage of red blood per rectum, it is likely that the patient would be more unstable than the vignette describes. It is unlikely that an abdominal ultrasound would reveal the source of this bleeding. A Meckel scan could reveal the source of bleeding but should not be done until the patient is stable.
3.
(B)
The description of the bleeding could correspond to any of the entities listed. It is the remainder of the history and physical examination that reveals the answer. Meckel diverticulum causes significant bleeding in this age group. It is often painless (see
Figure 48-1
). A juvenile polyp does not cause significant blood loss and is not associated with hemodynamic instability. Intussusception is usually associated with cramping abdominal pain before bloody stool. A small percentage of children with intussusception present with extreme lethargy, pallor, and heme-positive stools. Infectious colitis causing this amount of bleeding would be associated with cramping abdominal pain and diarrhea.

FIGURE 48-1.
Meckel’s diverticulum. This intraoperative photograph shows Meckel’s diverticulum in ileum that has been eviscerated. (Reproduced, with permission, from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery, 9th ed. New York: McGraw-Hill; 2010: Fig. 28-23.)
4.
(C)
5.
(C)
See explanation for answer 3.
6.
(A)
7.
(E)
If the intussusception is reduced surgically, the rate of recurrence is 2-5%. If the intussusception is reduced with a contrast enema, the chance of recurrence is 10% (see
Figure 48-2
).
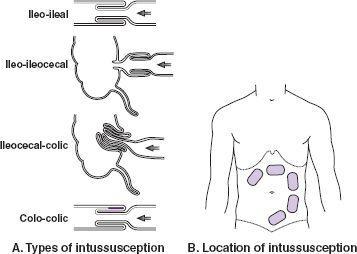
FIGURE 48-2.
Intussusception. This is the prolapse of one segment of intestine into an adjoining segment.
A.
The four types of intussusception: The enfolding of the lumen is in the direction of fecal flow, as shown by the arrows. In the intracolic type, the stippling indicates a neoplasm that is usually the cause of the telescoping.
B.
Locations: The usual sites of palpable masses are shown as sausage-shaped outlines; these are usually in the colon. (Reproduced, with permission, from LeBlond RF, DeGowin RL, Brown DD. DeGowin’s Diagnostic Examination, 9th ed. New York: McGraw-Hill; 2009: Fig. 9-33.)
8.
(B)
Painless bright blood per rectum in this age group is likely because of a juvenile polyp. Most present between the ages of 2 and 10 years. They are unlikely to cause significant blood loss or other serious symptoms.
9.
(C)
There is no increased chance of malignancy associated with a solitary juvenile polyp. The risk is higher in patients who have 3 or more polyps. The risk is not related to family history.
10.
(A)
Several syndromes are associated with multiple polyps throughout the colon. Familial adenomatous polyposis coli (FAP) is an autosomal dominant condition characterized by large numbers of adenomatous (premalignant) lesions throughout the colon. The cause is a mutation in the tumor suppressor gene
APC
. These patients are at risk for colon cancer in the third decade of life. Definitive treatment is prophylactic colectomy. Mutations in the
APC
gene are responsible for Gardner syndrome (multiple colorectal polyps, osteomas, lipomas, fibromas epidermoid cysts, and dermoid tumors). APC mutations are responsible for some cases of Turcot syndrome (primary brain tumor and multiple colonic polyps). Peutz-Jeghers syndrome is a distinct disease caused by a rare autosomal dominant mutation characterized by mucosal pigmentation of the lips and gums and hamartomas throughout the GI tract. Symptoms include GI bleeding and cramping, abdominal pain, and obstruction because of intussusception. Cancer develops in 50% of patients. Colorectal, breast, and gynecologic tumors occur most frequently (see
Figure 48-3
).
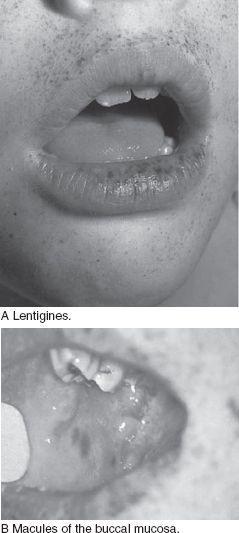
FIGURE 48-3.
Peutz-Jeghers syndrome.
A.
Lentigines, which are dark brown to gray-blue, appear on the lips, around the mouth, and on the fingers. Lip macules may, over time, disappear.
B.
Macules of the buccal mucosa are blue to blue-black and are pathognomonic; unlike lip lesions, these do not tend to disappear with time. (Reproduced, with permission, from Wolff K, Goldsmith LA, Katz SI, et al. Fitzpatrick’s Dermatology in General Medicine, 7th ed. New York: McGraw-Hill; 2008: Fig. 73-18A, B.)
11.
(A)
See above.
12.
(D)
Same explanation as for question 1.
13.
(E)
Of course, the first step is to fluid-resuscitate the child. In this child there is an upper GI bleed with hemodynamic instability. This is very unusual for a 4-year-old. The nasogastric lavage will allow you to determine whether there is continued bleeding. There is a possibility that this could be a variceal bleed, so it is important to check liver numbers and function (especially PT).
14.
(A)
Peptic ulcer disease is the most common cause of upper GI bleeding in a 4-year-old. It would be unlikely for a 4-year-old to have an
H pylori
infection causing a GI bleed. GERD would have long-standing symptoms. Swallowed epistaxis is unlikely to cause hemodynamic changes in an otherwise healthy individual. Bleeding from esophageal varices would be associated with liver disease or portal vein thrombosis. Both are rare in this age group.
15.
(C)
Mallory-Weiss tears occur after several episodes of vomiting. The tear usually occurs in the gastroesophageal junction. In children the bleeding is usually self-limited (see
Figure 48-4
).
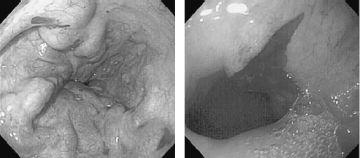
FIGURE 48-4.
Mallory-Weiss tear at the gastroesophageal junction. (Reproduced, with permission, from Fauci AS, Kasper DL, Braunwald E, et al. Harrison’s Principles of Internal Medicine, 17th ed. New York: McGraw-Hill; 2008: Fig. 285-18.)
16.
(D)
In developing countries,
H pylori
infections occur later in childhood. In the United States, the rate of infection in lower socioeconomic groups is much higher than for the population as a whole. GERD would be expected to have more symptoms. Herpetic esophagitis is very rare in immunocompetent hosts.
17.
(D)
Several tests are available to diagnose
H pylori
. Endoscopic mucosal biopsy is the most sensitive. The
H pylori
bacteria produce the enzyme urease. Christensen urea medium (CLO test) has a color change if
H pylori
is present in a biopsy specimen. Detection of serum IgG antibodies is sensitive and specific if done correctly. The sensitivity varies among commercial laboratories. Stool antigen tests are available but have lower sensitivity. Treatment consists of a proton pump inhibitor, clarithromycin, and amoxicillin or metronidazole.
18.
(E)
A small firm liver with a large spleen is characteristic of cirrhosis with portal hypertension. The bleeding can come from esophageal varices or gastropathy. The patient’s coagulopathy (from liver disease) and thrombocytopenia (from hypersplenism) must be corrected to stop the bleeding. Somatostatin infusions decrease the pressure in the splanchnic vascular bed and decrease portal pressure. The final treatment is an endoscopic procedure to determine the source of the bleeding and treat the varices. The most common treatments are banding and sclerotherapy. A variceal bleed can be a lifethreatening event, and more than 1 treatment modality may be necessary to treat it.
 S
S
UGGESTED
R
EADING
