Pediatric Examination and Board Review (125 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

FIGURE 75-1.
Bacterial vaginosis. Clue cells are large epithelial cells covered with bacteria. (Reproduced, with permission, DeCherney AH, Nathan L. Current Diagnosis & Treatment: Obstetrics & Gynecology, 10th ed. New York: McGraw-Hill, Fig. 37-4.)
9.
(E)
Although trichomoniasis has already been confirmed on wet prep and herpes simplex infections is very likely from a clinical standpoint, concomitant bacterial cervicitis and/or UTI still need to be excluded. In several clinical series, concurrent UTI and genital infections were found in up to 20% of adolescent girls presenting with genitourinary symptoms.
10.
(B)
Even though the clinical picture is highly suggestive of vulvovaginitis and cervicitis, a urine culture will help rule out concomitant UTI. HIV and syphilis testing should be done in all patients with evidence of other STDs. A pregnancy test will be needed, given this patient’s history of unprotected intercourse.
11.
(D)
An estimated 3 million teenagers acquire an STD every year, with an approximate rate of 1 in 4 sexually active teens between the ages of 13 and 19 years. Approximately two-thirds of all cases of STDs occur in people younger than 24 years. A chlamydial infection is the most common bacterial STD at all ages. Forty percent of chlamydial infections occur in young women 15-19 years of age. In adolescent girls in this age group, the rate of chlamydial infections is 3.5 times higher than that of gonorrhea. Both chlamydia and gonorrhea have a predilection for columnar epithelium. The high prevalence of these infections in young women may be explained, at least in part, by the presence of cervical ectopy, a normal developmental finding during adolescence. It is estimated that more than 50% of females and 25% of males with chlamydial infections may be asymptomatic. Test of cure after treatment for chlamydia is only recommended if the patient is pregnant, symptoms persist after treatment, or compliance with the medication regimen is doubted. According to present CDC recommendations, all sexually active adolescent girls should be screened for
C trachomatis
infection every 6 months.
12.
(B)
As many as 50% of women and most men with trichomonal infections are asymptomatic. For those adolescent girls who present with symptoms, vaginal discharge and itching are the most common complaints. The discharge is typically yellow green and may be frothy. On physical examination, vulvar and vaginal erythema are common and a “strawberry cervix,” resulting from swollen papillae and punctuate hemorrhages, may be present. Trichomonads can be detected on wet mounts (with 50-70% sensitivity) (see
Figure 75-2
). Cultures and DNA amplification methods increase sensitivity to 97% and 99%, respectively. Partners of patients with a
Trichomonas
infection should also be treated.
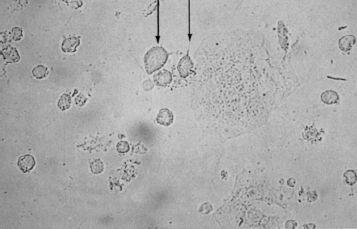
FIGURE 75-2.
Trichomonas. Saline wet mount demonstrating oval-bodied, flagellated trichomonads (see arrow). They are similar in size to leukocytes and can be distinguished from them by their motility and presence of flagella. (Reproduced, with permission, from Handsfield HH. Atlas of Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
13.
(C)
A first episode of primary genital herpes infection is defined as an infection in a patient with no prior history of genital herpes who is seronegative. The incubation period is about a week with a range of 2-12 days. Vesicular lesions subsequently appear, marking the end of the incubation period. The vesicles then evolve into ulcers that may coalesce and the virus may shed for at least 10-12 days. Reepithelization takes place in 2-3 weeks and leaves no scarring. Cervicitis is common in 70-90% of first episodes but is less common in recurrent disease. Recurrent genital herpes infections are usually milder, have less constitutional symptoms, present with fewer lesions, and heal faster. During recurrent infections viral shedding lasts for about 4 days. Up to 15% of genital herpes infections are caused by HSV-1.
14.
(B)
The Tzanck preparation, in which scrapings from a lesion are stained with Wright stain, may show characteristic multinucleated giant cells (see
Figure 75-3
). The Pap smear would show the same findings with a 60-70% sensitivity and 95% specificity. Colposcopy may reveal characteristic ulcers with a sensitivity of about 70%. Viral cultures are the test of choice for confirmation of infection. Virus detection, however, depends on the stage of the lesions: Cultures are positive in 90% of vesicles and 70% of ulcers but only on 25% of crusted lesions.
15.
(C)
The incubation period of gonorrhea is 3-5 days. It is estimated that 75-90% of women and 10-40% of men infected with gonorrhea are asymptomatic. Screening for gonorrhea in asymptomatic girls can be accomplished by obtaining a urine nucleic acid amplification techniques (NAAT) test or an endocervical sample for culture. Routine cultures from the pharynx and rectum in adolescents are not cost effective in asymptomatic adolescents. The currently recommended treatments are believed to be effective in gonorrhea eradication from all sites.

FIGURE 75-3.
Herpes simplex virus: positive Tzanck smear A giant, multinucleated keratinocyte on a Giemsa-stained smear obtained from a vesicle base. Compare the size of the giant cell to that of the neutrophils also seen in this preparation. (Reproduced, with permission, from Wolff K, Johnson RA. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology, 6th ed. New York: McGraw-Hill; 2009: Fig. 27-27.)
16.
(E)
PID comprises a variety of inflammatory disorders of the upper genital tract in women, including endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. It is a common condition that affects 1 million women and leads to 200,000 hospitalizations per year. Seventy-five percent of women with PID are younger than 25 years. In a quarter of affected women, PID leads to sequelae such as infertility, ectopic pregnancy, and chronic pelvic pain. Teenagers account for a fifth of all cases of PID. PID is thought to be polymicrobial, caused by aerobic and anaerobic bacteria, and results from ascending infection of bacteria from the cervix. Among the sexually transmitted infections, gonorrhea, chlamydia, and genital mycoplasma, are the most common pathogens responsible for PID. Smokers have twice the rate of nonsmokers, and there is also increased risk for PID among IUD users. The use of barrier methods and birth control pills lowers the risk for PID.
17.
(B)
The diagnosis of PID relies heavily on clinical judgment. Because of the lack of conclusive diagnostic indicators, the condition is correctly diagnosed on clinical and laboratory grounds in 65% of cases. The differential diagnosis is extensive and includes appendicitis, gastroenteritis, irritable bowel syndrome, cholecystitis, endometriosis, hemorrhagic ovarian cyst, ovarian torsion, nephrolithiasis, and somatization. The most frequently found clinical features are abdominal pain (100%), adnexal tenderness (90%), and cervical motion tenderness (80%). Vaginal discharge, abdominal guarding, and rebound are less common (73% and 61%, respectively). Fever is present in only 30% of cases. Minimal diagnostic criteria include abdominal pain, adnexal tenderness, and cervical motion tenderness. Fever and vaginal discharge are additional clinical features that may be helpful when present. An increased ESR, CRP, and laboratory documentation of cervical infection with gonorrhea or chlamydia will provide supportive evidence. Additional tests, such as pelvic ultrasound, are helpful to detect a pelvic abscess or an ectopic pregnancy. A pregnancy test will be needed as part of the workup.
Empirical treatment is started as soon as the diagnosis of PID is suspected. Although most women with PID are treated in the outpatient setting, adolescents may need to be hospitalized for treatment, given their often unpredictable compliance. Other indications for inpatient treatment include pregnancy as well as suspected surgical emergencies such as appendicitis, ectopic pregnancy, or pelvic abscess. Severe illnesses with nausea or vomiting also preclude outpatient management. Careful follow-up is required in all cases.
18.
(C)
Your findings so far confirm the diagnosis of trichomoniasis and are also highly suggestive of a first episode of genital herpes. Concurrent gonorrhea and/or chlamydia are also likely in this adolescent at risk who presents with mucopurulent cervicitis. All these infections will need to be treated to avoid short- and long-term complications. Although you could treat her for trichomonas and herpes on the first visit and ask her to return for treatment of gonorrhea and chlamydia once these infections are confirmed, follow-up may be unreliable in view of this patient’s psychosocial history. Thus it would be preferable to treat her for all suspected infections on the present visit. Antibiotic resistance has been a major problem in the treatment of gonorrhea. The 2010 CDC guidelines for the treatment of STDs state that resistance to quinolones (ciprofloxacin and ofloxacin) precludes their use in certain areas of the country, particularly in the western United States. The recommended dose of ceftriaxone for the treatment of uncomplicated gonorrhea cervicitis is 125 mg IM single dose. Regimens that include ceftriaxone or doxycycline also cover incubating syphilis. Azithromycin, doxycycline, and erythromycin will all be effective in treating chlamydia. However, azithromycin is a preferred treatment in adolescents because of its easy one time dose schedule. Several antiviral agents are available for the treatment of the first episode of genital herpes. Among them, valacyclovir is the one that requires the least frequent dosing, increasing the potential for compliance. Many experts do not prescribe antivirals for uncomplicated herpes infection. Ciprofloxacin has not been approved for patients younger than 18 years.
19.
(E)
This patient’s sexual partner should be treated for trichomonas, chlamydia, and gonorrhea infections. HIV and RPR testing is recommended, and the patient is advised to abstain from sexual activity until all her lesions are healed. Underlying her presenting concerns, this 14-year-old has a host of risk factors, including school failure, high risk for pregnancy and STDs, runaway behavior, and drug use. A brief initial discussion at this visit will need to be followed up with more extensive evaluation and interventions including individual and family counseling.
 S
S
UGGESTED
R
EADING
