Oxford Handbook of Midwifery (114 page)
Read Oxford Handbook of Midwifery Online
Authors: Janet Medforth,Sue Battersby,Maggie Evans,Beverley Marsh,Angela Walker

- Before modern times, LAM was the only contraceptive method available, and is still the only method available to women in many parts of the world.
Additional contraception
- Many women choose to rely on an additional method, such as the condom or the progesterone-only pill (POP).
- If the mother is using the a POP while fully breastfeeding, it is unnecessary to give emergency contraception if a pill is missed.
- If a breastfeeding mother chooses a POP, the amount passed to the baby in the breast milk is the equivalent of one POP in 2 years, considerably less progesterone than in formula milk.
2 - As soon as the baby begins to be weaned or the mother has a period, it is important that, if she wants effective oral hormonal contraception, she is switched to desogestrel 75micrograms or the combined contraceptive pill.
Return of ovulation
- The time taken for return of ovulation depends on the frequency, intensity, and duration of feeding, maintenance of night feeds, and introduction of supplementary feeding.
- Midwives should be confident in recommending this method to mothers,
provided the criteria are met
.
LACTATIONAL AMENORRHOEA METHOD
529
Ask the mother:
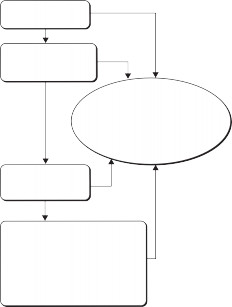
Is your baby less
NO
than 6 months old?YES
Are you amenorrhoeic?
NO
(no vaginal bleeding after56 days postpartum)
YES
The mother’s chance of pregnancy is increased. She should not rely on breastfeeding
alone. Use another family planning method, but continue to breast feed for the child’s health
Are you fully or nearly
NO
fully breastfeedingyour baby? YES
THERE IS ONLY ABOUT A 2%
 CHANCE OF PREGNANCY
CHANCE OF PREGNANCYShe does not need a complementary family planning method at this time. HOWEVER: Tell the mother when the answer to any one of these questions becomes NO...
Fig. 22.1
Lactational amenorrhoea method of contraception.Reprinted by permission of Fertility UK from M www.fertility.uk.org.
- World Health Organization (1999). Multinational study of breast feeding and lactational amenor- rhoea method. III Pregnancy during breastfeeding.
Fertility and Sterility
72
(3), 431–40. - Guillebaud J (2008).
Contraception Today
, 6th edn. London: Taylor and Francis.CHAPTER 22
Contraception530
Combined oral contraceptive: ‘the pill’
Contents
Each tablet contains a combination of oestrogen and progesterone. Most brands contain 30–35micrograms of ethinylestradiol and a progestogen.
In the UK, the combined oral contraceptive pill is the most commonly used form of contraception:
- It is highly effective
- It is convenient
- It is not related to intercourse
- It is reversible
- It reduces the incidence of ectopic pregnancy
- It results in lighter and less painful periods
- It possibly helps to reduce premenstrual symptoms
- It protects against ovarian and endometrial cancer.
When is it taken?
- Ideally, the woman should start the first pack on the first full day of menstrual bleeding and definitely within the first 5 days of the cycle. If this is done, then follicle stimulating hormone (FSH) inhibition will be complete for that cycle, and no additional contraception will be
 necessary.
necessary. - If the pill is started later than the 5th day of the cycle, she should use a
condom every time sexual intercourse occurs in the next 7 days. After that the hormonal control will be established.
- It is not started in the latter half of the menstrual cycle, because of the risk of pregnancy.
- Tell the woman to take one pill daily, at approximately the same time every day, choosing a time of day that is most convenient and best remembered. She should follow the arrows on the pack until all
21 pills have been taken. Then she will have a 7-day break, during which a withdrawal bleed, ‘period’, will occur. The next pack should be commenced 7 days later.
Follow-up
- Normally, the first prescription is for 3 months, with an appointment to return to clinic in 8–10 weeks for review.
- Unless there any menstrual irregularities or other side-effects are evident, follow-up and repeat prescription is then 6–12 months, depending on local policy.
Points to remember
- A useful tip for an effective pill-taking regimen is to ask the woman to make a note of the day she started the pill for the first time: that is the day she will always start a new pack.
- She should make a note of the new pack start date. Again, a paper diary, electronic diary, or mobile phone calendar and alarm can be used.
- It is highly effective
COMBINED ORAL CONTRACEPTIVE: ‘THE PILL’
531
- Before modern times, LAM was the only contraceptive method available, and is still the only method available to women in many parts of the world.
- Missed pill: there is a ‘window’ of 12h, during which a pill may be taken later than normal and still be within the normal regimen. If more than 12h late, then advise her to follow the regimen given in b When the pill may not be effective, p. 532.
- If the woman smokes, she must be warned of the increased risk of coronary heart disease and venous thromboembolism.
- After giving birth:
- Ideally the combined pill should not be started until at least 21 days after birth, to allow the body to recover physiologically from birth and to avoid increasing the thrombo-embolic risk.
- However, there are some women for whom the risk of further pregnancy is high and who need highly effective contraception. In this case, refer the woman to the contraception and sexual health clinic for appropriate management.
- The combined pill should never be given to a breastfeeding mother, as the oestrogen component will suppress her lactation within 24–48h.
- If a breastfeeding mother requires hormonal contraception, then advise a progesterone-only method.
- If the combined pill is started while the mother still has a vaginal blood loss, the progesterone component will cause bleeding to
become heavier and more prolonged. Be aware of this and also
 warn the mother.
warn the mother. - The combined pill should be avoided, wherever possible, in a mother who has reduced mobility following birth, e.g. after
caesarean section, because of the increased thrombo-embolic risk.
- Ideally the combined pill should not be started until at least 21 days after birth, to allow the body to recover physiologically from birth and to avoid increasing the thrombo-embolic risk.
- Blood pressure and personal and family medical history are checked annually for any significant changes that may signal caution or discontinuation of this method of contraception, notably cardiovascular issues such as hypertension, heart attacks, and stroke or thrombo-embolic disorders.
CHAPTER 22
Contraception532
When the pill may not be effective
Missed pill(s)
The WHO
1
issued new missed pill guidance in 2004, which was adapted for UK use in 2005
2
(see Fig. 21.2):- If the pill for that day is taken more than 12h late, advise the woman to take the missed pill as soon as it is remembered and take the next
scheduled pill at its normal time. In practice, what often happens is that two pills are taken together.
- Up to two pills can be missed anywhere in the pack (only one if taking Loestrin
®
20, Mercilon
®
, or Femodette
®
). No additional contraception is needed. - If three or more pills are missed (two if taking Loestrin
®
20, Mercilon
®
, or Femodette
®
). Take the last pill missed as soon as it is remembered. Leave any earlier missed pills in the pack. Use an extra method of contraception for the next 7 days (the male condom is the easiest). - If three or more pills have been missed and the woman has had unprotected sex in the last few days, advise her to consider emergency contraception, as she may be at risk of pregnancy.
- If seven or more pills are left from now until the end of this cycle: she should continue taking the pill in the normal way to the end of the pack
 and have the normal 7-day break. The normal period should occur.
and have the normal 7-day break. The normal period should occur. - If fewer than seven pills are left from now until the end of this cycle: she should continue to the end of the pack, but not have the 7-day break. Tell her to start the new pack immediately and follow the normal daily regimen to complete the pack in the normal way. In this case there will be no period between the two packs, but there should be a normal period at the end of the second pack.
Points to remember
- She should only take one missed pill. If more than one pill has been missed, advise her to leave the other missed pills in the pack. If this happens, it is important that a condom is used for every act of sexual intercourse for the next 7 days.
- 2 When a pill has been missed for more than 12h in a cycle, the risk of pregnancy is increased. Any disturbance in menstrual cycle as a result should be followed up with a pregnancy test.
Antibiotic therapy
The well-established guidance that the use of additional precautions must be used when taking any broad spectrum antibiotic has changed, in the light of worldwide research evidence, and is no longer the case.
4
This also applies to fluconazole, used in the treatment of
Candida
(‘thrush’).Antiretroviral therapy
Drug interactions between the antiretroviral drugs and the combined hormonal contraceptive may alter the effectiveness of the combined hor- monal contraceptive and consistent additional use of the condom should be recommended.
3WHEN THE PILL MAY NOT BE EFFECTIVE
533
Nausea and vomiting
If the woman vomits within 3h of taking the pill, she may not have absorbed sufficient amounts of the oestrogen component to suppress ovulation effectively. In this case a condom should also be used for every act of sexual intercourse for the duration of the episode of illness involving vom- iting and for the next 7 days, to allow the contraceptive effect to return.
How many pills have you missed?*
Take the last pill you missed now. Take the rest of the pack as usual. Leave the earlier missed pill.
No additional contraception needed.
anywhere in the pack (only
one
if taking the pills Loestrin
®
20, Mercilon
®
or Femodette
®
).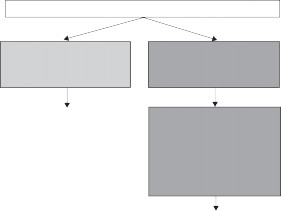
Three or more,
(
two
if taking the pills Loestrin
®
20, Mercilon
®
or Femodette
®
).Take the last pill you missed now
 Take the rest of the pack as usual.
Take the rest of the pack as usual.Leave any earlier missed pills.
Use an extra method of contraception for the next seven days.
If you have had unprotected sex in the previous few days, you may need emergency contraception. Seek advice.
How many pills are left in the pack after the missed pill?
Seven or more
Less than seven
Finish pack, have the usual seven day break or take the placebo tablets.
Finish pack and begin new one the next day.
(This means missing out the break or not taking the placebo tablets.)
- If you miss pills and have also missed pills in your previous packet, speak to your doctor or nurse as you may need emergency contraception.
Fig. 22.2
Missed pill guidance.Copyright © fpa 2007, reprinted by permission of the publisher.
CHAPTER 22
Contraception534
Drug interactions
Certain drugs may inhibit absorption/reduce the effectiveness of the pill, so it is imperative that you check whether or not the woman is taking any other medication when discussing possible use of the pill.
4The main interacting drugs are:
- Enzyme-inducing anticonvulsants used in the treatment of epilepsy, tuberculosis, and HIV.
- Drugs used in the treatment of TB.
- Coumarin anticoagulants (e.g. warfarin).
- St John’s wort (a herbal complementary medicine often taken by women).
- Enzyme-inducing anticonvulsants used in the treatment of epilepsy, tuberculosis, and HIV.
Refer the woman to the contraception and sexual health clinic or general practitioner for review of the drug regimen. Advise her that St John’s wort must not be taken when using combined hormonal contraception.

- World Health Organization (2004).
Selected Practice Recommendations for Contraceptive Use
. Geneva: WHO. - Faculty of Family Planning and Reproductive Health Care (2005).
Faculty Statement: Missed Pills: New Recommendations
. London: FFPRHC. - Faculty of Sexual and Reproductive Health Care (2009).
UK Medical Eligibility for Contraceptive Use
. London: Faculty of Sexual and Reproductive Health Care. Available at: M www.ffprhc.org.uk/
admin/uploads/UKMEC2009.pdf (accessed 10.4.10). - Faculty of Sexual and Reproductive Health Care (2011).
Drug Interactions with Hormonal Contraception
. London: FSRSH. Available at: M www.ffprhc.org.uk/admin/uploads/ CEUGuidanceDrugInteractionsHormonal.pdf
CONTRACEPTIVE PATCH
535
Contraceptive patch
The ‘pill in a patch’ first became available in the UK in 2003. It is a combi- nation oestrogen and progesterone drug and can be given to any woman who is suitable for the combined pill. Each pack contains 3 months’ supply.
Using the patch
The woman should:
- If you miss pills and have also missed pills in your previous packet, speak to your doctor or nurse as you may need emergency contraception.
- If the pill for that day is taken more than 12h late, advise the woman to take the missed pill as soon as it is remembered and take the next
Other books
The Carnelian Legacy by Cheryl Koevoet
Delayed Death (Temptation in Florence Book 1) by Boeker, Beate
Real Peace by Richard Nixon
Cricket XXXX Cricket by Frances Edmonds
Ravished by Amanda Quick
The Mystery of the Zorse's Mask by Linda Joy Singleton
The Alchemist's Key by Traci Harding
Aces by T. E. Cruise
White Oblivion by Amirah Bellamy
