Murder and Mayhem (17 page)
Authors: D P Lyle

Over several days to a week your character could gradually become fatigued, gain several pounds in weight (as the body holds on to salt in water), become progressively short of breath, develop swollen ankles, and have to be admitted to the hospital for treatment.
If you want your young lady to be at home, go with premature labor. If you want her in the hospital, any of these would work.
What Medical Emergency Would Expose a Young Woman's Secret Pregnancy?
Q: In my story a sixteen-year-old girl attempts to hide her pregnancy from her parents and is successful for several
months. At that time I would like for her secret to be discovered in some way that would be dramatic and threatening to her life. I thought about a miscarriage, but could you suggest any other situations that would put her life in danger? I want her to survive but just be scared.
A: Several situations come to mind.
A miscarriage, as you suggested, would work well. It could occur in a single dramatic event or progress over several days in a stuttering fashion. She could suddenly develop severe lower abdominal cramping pain with bleeding and expulsion of fetal tissues. If she was several months along, a formed fetus would appear. She could collapse and sink into a state of shock, manifested by low blood pressure, a pale appearance with perhaps a bluish tinge to her fingers and toes and around her lips, and a cold, clammy sweat. She would be taken to the hospital emergency room, where IVs would be started and blood and fluids given, and then she would be taken to surgery for an emergency D and C. In this procedure the physician, likely a gynecologist, would remove any retained tissues from the uterus.
Alternatively, she could develop episodic pains, with or without vaginal bleeding or spotting, which would progress until the miscarriage occurred. A visit to the hospital and a D and C would follow. In either circumstance, she would remain in the hospital for a few days but would likely recover completely without any long-term problems—at least, physical problems. Her psychological reactions could be long term and significant.
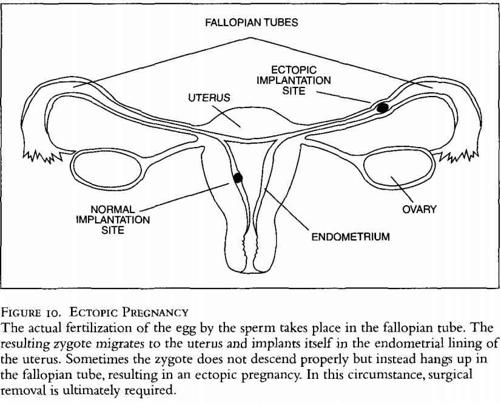
Another possibility would be an ectopic pregnancy. During fertilization the egg leaves the ovary, finds its way to the mouth of the fallopian tube, and begins to descend toward the uterus. The sperm enter the cervical os (the opening at the end of the cervix) and swim through the cervix and into the uterus. They then migrate up the fallopian tube, where they meet the descending egg. One
wins the race, and the actual fertilization takes place within the fallopian tube. The fertilized egg continues downward and into the uterus, where implantation in the endometrium, which lines the uterine wall, occurs and the pregnancy commences.
Sometimes the fertilized egg gets hung up in the fallopian tube (Figure 10). The zygote (the ball of cells that will grow into the fetus) develops normally and continues to enlarge just as it would in the uterus. Early on, the mother's symptoms would be exactly the same as if she had a normal intrauterine (inside the uterus) pregnancy. She may suffer morning nausea, mood swings, breast tenderness, and all the other symptoms of pregnancy. Testing for pregnancy would be positive, and no one would know or suspect that anything was wrong. As the fetus develops and grows, however, the fallopian tube, unlike the uterus, cannot expand to accommodate the enlarging fetus. Ultimately, the fallopian tube ruptures. This may take six to twelve weeks.
The symptoms are similar to a miscarriage except the abdominal pain may be more severe and in the right or left side of the lower abdomen, depending on which tube held the ectopic pregnancy, rather then centralized in the mid portion of the lower abdomen. Vaginal bleeding may be much less dramatic or may not occur at all, since the ruptured fallopian tube would bleed into the abdominal cavity and the uterine os would not likely open to allow passage of blood as it does in a miscarriage.
An ectopic pregnancy typically causes abdominal pain on the right or left side for several days before it ruptures. It is often confused with appendicitis, since the symptoms are similar. A pelvic exam usually reveals a palpable mass in either the right or left lower abdomen in the area of the fallopian tubes and ovaries—an area called the adnexa. If she saw her gynecologist at this stage, he would determine that she had a positive pregnancy test and a tender adnexal mass, and would likely obtain an abdominal ultrasound (a picture of the abdominal contents using sound waves) and make
the diagnosis of an ectopic pregnancy. Surgery would follow. The affected fallopian tube would be removed. She could still have future pregnancies since the other tube, the ovaries, and the uterus would remain intact.
If she ignored or denied the abdominal pain, it would progressively become more severe and more frequent, but vaginal bleeding or spotting would be unlikely. Eventually, tubular rupture would occur.
Another scenario is that her fear of discovery would lead her into the hands of an unlicensed and unscrupulous clinic where abortions are done, no questions asked—for a hefty fee, of course. Here an unqualified physician or nurse or someone with no medical training at all would perform a makeshift D and C using improper equipment and with poor, if any, sterile technique. The life-threatening complications that might follow are many and severe.
She could continue to bleed from trauma that occurred during the procedure or from retained tissues, if the D and C was incomplete. Pain and bleeding would continue over several days, she would become progressively weaker and more anemic, and her secret would likely be discovered.
She could suffer a perforation of the uterus, a common occurrence in the days of coat hanger abortions. Here, the instrument used to clean out the unwanted pregnancy pushes through the uterine wall and into the abdomen. The uterus is actually perforated quite easily, and physicians performing therapeutic abortions or D and C's are very cognizant of this fact and take great care to avoid this complication. This is a very painful event and leads to severe bleeding and shock. Death is common, since the uterus tends to bleed a great deal when damaged in this manner. Emergency surgery for repair or removal of the uterus would be lifesaving.
She could survive the abortion only to develop an infection several days later. Infections within the uterus are particularly treacherous. The uterus has little capacity to contain infections, and, thus, any bacterial organisms introduced into the uterine cavity by improper sterile technique quickly enter the bloodstream and lead to septicemia (bloodstream infection) and septic shock. Septic shock occurs when the toxins of the bacteria cause severe derangements in the cardiovascular controls of blood pressure and the ability of the body's tissues to use oxygen. The symptoms and signs of septic shock include low blood pressure, high temperatures, shaking chills, confusion, disorientation, and ultimately death. This type of infection has a high mortality rate. Surgical removal of the uterus, high doses of antibiotics, intravenous steroids, and drugs to support the blood pressure are needed if survival is to be realized (dopamine, epinephrine, and Dobutamine are commonly used intravenous agents for this purpose).
What Is the Gulf War Syndrome?
Q: I need some information about the Gulf War Syndrome for a short story I am writing. Everything I've read is confusing, and there seems to be a great debate as to whether it is real or not. Is it? What causes it, and how does it affect the people who have it? Is there any treatment for it?
A: Your confusion is justified. Even the experts argue over whether it is real and, if so, what its causes are. It is a broad and complex subject, and our understanding of the syndrome is in a state of evolution.
The controversy began when many members of our military who returned from the Persian Gulf War began to exhibit unusual symptoms. The most common were fatigue, headaches, memory loss, insomnia, various rashes, swelling and burning of the feet and hands, joint pain and swelling, chronic cough, muscular weakness, loss of coordination, numbness and tingling in their extremities, rectal bleeding, and cardiac arrhythmias with palpitations. This constellation of symptoms became known as the Gulf War Syndrome (GWS).
In medicine the term "syndrome" refers to a group of signs and symptoms that occur together often enough to be recognized as a distinct entity but for which no causal or physiologic relationship has been established. If a man and a woman are walking down the street holding hands, it doesn't mean they are married. In a syndrome the signs and symptoms hold hands, but marriage or any other relationship between them has not been scientifically established. This is the case with GWS.
The cause of GWS is unknown. Some feel it is entirely psychosomatic, while others suggest it is from chemical or biologic weapons
used by the Iraqi military or it is the result of our destruction of their chemical weapons bunkers, which released the agents into the air and exposed our troops to the toxic vapors. Still others believe it is related to the vaccines against anthrax and botulinum that our soldiers received or perhaps to the pyridostigmine bromide pills that were given to counteract the effects of many known chemical weapon compounds. The most likely explanation may be a combination of all these. That is, the toxic symptoms may result from a mixture of vaccines and medicines that the soldiers were given and the chemical and/or biologic agents to which they were exposed.
Toxic chemicals that the Iraqi military possessed at that time include sarin, Soman, Tabun, VX, hydrogen cyanide, cyanogen chloride, mustard gas, thiodiglycol (a precursor chemical of mustard gas), and Lewisite. Possible biologic agents include botulinus toxin and anthrax.
Sarin, Soman, Tabun, and VX are powerful neurotoxins that act quickly and damage the neurologic system of those who are exposed. Since many of the symptoms of GWS are neurologic in nature, these chemicals could easily be involved. Mustard gas, thiodiglycol, cyanogen chloride, and Lewisite can damage the skin and lungs. The botulinus toxin and anthrax can cause severe neurologic defects. The vaccines mentioned above as well as pyridostigmine bromide have neurologic side effects.
Unfortunately, a great deal of what is believed, suggested, or speculated to be the cause of GWS has little if any scientific support—not yet, anyway. Research in this area is ongoing. While we await a better understanding of this syndrome, no cure or effective treatment is available.
THE EFFECTS OF GUNS, KNIVES, EXPLOSIVES, AND OTHER WEAPONS OF DEATH
Can a Stun Gun Serve as a Murder Weapon?
Q: I'm working on a story that requires one man to kill another while both are in a crowd of people. My thought is that the killer uses a stun gun. While these devices are not supposed to be fatal, is it possible that death could result from the application of a longer-than-usual dose of electricity if the victim has a heart condition or pacemaker?
