How Doctors Think (38 page)
Authors: Jerome Groopman

Arthur Elstein, as mentioned earlier, is one of the pioneers in the field of medical decision-making. His book edited with Jack Dowie presents a remarkable range of opinions on the subject and is well worth consulting for those who wish to learn more:
Professional Judgment: A Reader in Clinical Decision Making
(Cambridge: Cambridge University Press, 1988). The quotes from Donald A. Schön are from "From technical rationality to reflection-in-action," in
Professional Judgment,
pp. 60–77. The quote from David Eddy of Duke University is from "Variations in physician practice: The role of uncertainty," in
Professional Judgment,
pp. 4559. Similarly, the chapter by Jay Katz refers to the work of Renée Fox on uncertainty and describes Katz's own experiences during his medical training: "Why doctors don't disclose uncertainty," in
Professional Judgment,
pp. 544–565.
7. Surgsery and Satisfaction
"The best doctors in...": see, again, Kent Sepkowitz, "A few good doctors: Don't look for them on a magazine top-10 list,"
Slate,
June 13, 2006.
Richard Selzer's book
Letters to a Young Doctor
(New York: Simon and Schuster, 1982) is a wonderful collection and worth reading for both the general reader and professionals. Dr. Sherwin Nuland writes beautifully about the experience of the seasoned surgeon in
How We Die: Reflections on Life's Final Chapter
(New York: Knopf, 1994), and
How We Live
(New York: Vintage, 1998). For those interested in the perspective of a surgical resident in training, see a book by my colleague at
The New Yorker
Atul Gawande,
Complications: A Surgeon's Notes on an Imperfect Science
(New York: Metropolitan Books, 2002). Dr. Light's comments about every patient coming in with a story might strike the reader as unusual, since surgeons are often depicted as being interested only in working with their hands. But as Roter and Hall said, the best ones have the full package.
Satisfaction of search as a cognitive error is well described in Pat Croskerry, "Achieving quality in clinical decision making: Cognitive strategies and detection of bias,"
Academic Emergency Medicine
9 (2002), pp. 1184–1204.
A terrific and amusing article about the world of orthopedics is Donald Berwick, "My right knee,"
Annals of Internal Medicine
142 (2005), pp. 121–125.
8. The Eye of the Beholder
A special issue of the
Journal of the American College of Radiology
(vol. 3, 2006) had a number of articles that provided considerable data and a bibliography for this chapter: Harold L. Kundel, "History of research in medical image perception," pp. 402–408; Craig A. Beam et al., "The place of medical image perception in 21st-century health care," pp. 409412; E. James Potchen, "Measuring observer performance in chest radiology: Some experiences," pp. 423–432; Elizabeth A. Krupinski, "Technology and perception in the 21st-century reading room," pp. 433–440; Matthew Freedman and Teresa Osicka, "Reader variability: What we can learn from computer-aided detection experiments," pp. 446–455; Bradley J. Erickson et al., "New opportunities in computer-aided diagnosis: Change detection and characterization," pp. 468–469; Dulia Ortega and César García, "Communication between radiologists and patients: An unsolved issue," pp. 472–477; Ehsan Samei, "Why medical image perception?," pp. 400–401.
The estimate of the number of cases being read by radiologists comes from Dr. Herbert Kressel, who served as the president of Beth Israel Deaconess Medical Center, Boston, in addition to being the Stoneman Professor of Radiology at Harvard.
The error rates in observing cyanosis, the misinterpretation of EKGs, and disagreement about cervical biopsies are from David Eddy, "Variations in physician practice: The role of uncertainty," in
Professional Judgment: A Reader in Clinical Decision Making,
ed. Jack Dowie and Arthur Elstein (Cambridge: Cambridge University Press, 1988), pp. 45–59.
There are numerous studies about the accuracy of mammography. Interested readers may consult the following to gain a sense of the data: Craig A. Beam et al., "Association of volume and volume-independent factors with accuracy in screening mammogram interpretation,"
Journal of the National Cancer Institute
95 (2003), pp. 282–290; Joann G. Elmore et al., "Variability in radiologists' interpretations of mammograms,"
NEJM
331 (1994), pp. 1493–1499; Yulei Jiang et al., "Potential of computer-aided diagnosis to reduce variability in radiologists' interpretations of mammograms depicting microcalcifications,"
Radiology
220 (2001), pp. 787–794; Daniel B. Kopans, "Mammography screening is saving thousands of lives, but will it survive medical malpractice?,"
Radiology
230 (2004), pp. 20–24.
More detail about Kundel's studies, particularly his seminal work, is found in his article in the
Journal of the American College of Radiology
cited above, as well as in G. Revesz and H. L. Kundel, "Psychophysical studies of detection errors in chest radiology,"
Radiology
123 (1977), pp. 559–562. Similarly, Ehsan Samei studied the challenge of detecting lung nodules: Ehsan Samei et al., "Subtle lung nodules: Influence of local anatomic variations on detection,"
Radiology
228 (2003), pp. 76–84.
Dr. Vickie Feldstein was a numbers whiz as a student, a valued member of the Newton South High School math team in Newton, Massachusetts. Her understanding of how to apply numbers to medical decision-making, as epitomized in this chapter, is a model for the modern physician who can look to metrics but also recognize their shortcomings.
An interesting paper about defensive medicine, meaning medical decisions made because of concerns about potential litigation, is David M. Studdert et al., "Defensive medicine among high-risk specialist physicians in a volatile malpractice environment,"
JAMA
293 (2005), pp. 2609–2617.
9. Marketing, Money, and Medical Decisions
There has been considerable controversy about the relationship among pharmaceutical companies, their educational programs, marketing to doctors, advertising to the public, scientific research, and clinical decisionmaking. Articles and books reflecting a diversity of opinion about these issues include Ashley Wazana, "Physicians and the pharmaceutical industry: Is a gift ever just a gift?,"
JAMA
283 (2000), pp. 373–380; Troyen A. Brennan et al., "Health industry practices that create conflicts of interest,"
JAMA
295 (2006), pp. 429–433; Jason Dana and George Loewenstein, "A social science perspective on gifts to physicians from industry,"
JAMA
290 (2003), pp. 252–255; David Blumenthal, "Doctors and drug companies,"
NEJM
351 (2004), pp. 1885–1890; Jerry Avorn,
Powerful Medicines: The Benefits, Risks, and Costs of Prescription Drugs
(New York: Knopf, 2004); Marcia Angell,
The Truth about the Drug Companies: How They Deceive Us and What to Do about It
(New York: Random House, 2004); Thomas Stossel, "Free the scientists!: Conflict-of-interest rules purport to cure a problem that doesn't exist—and are stifling medical progress,"
Forbes,
February 14, 2005; Thomas Stossel and David Shaywitz, "What's wrong with money in science?,"
Washington Post,
July 2, 2006; and an article by my colleague at
The New Yorker
Malcolm Gladwell, "High prices: How to think about prescription drugs,"
New Yorker,
October 25, 2004.
Robert Steinbrook highlighted drug companies' access to physicians' prescribing habits in "For sale: Physicians' prescribing data,"
NEJM
354 (2006), pp. 2745–2747, so now Karen Delgado and her colleagues no longer need to learn this information from readers of business magazines, like her husband.
Recently, practice guidelines that were written by a panel of experts were criticized because a drug company that made a questionable product recommended in the guidelines financially supported the writing: Peter Q. Eichacker et al., "Surviving sepsis—Practice guidelines, marketing campaigns, and Eli Lilly,"
NEJM
355 (2006), pp. 1640–1642.
The controversy over androgen replacement for aging men is nicely summarized in Paul M. Stewart, "Aging and fountain-of-youth hormones,"
NEJM
355 (2006), pp. 1724–1726, which was based on a recent study by K. Sreekumaran Nair et al., "DHEA in elderly women and DHEA or testosterone in elderly men,"
NEJM
355 (2006), pp. 1647–1659.
My article on
COX
-2 inhibitors was published in
The New Yorker
on June 15, 1998: "Superaspirin: A new kind of drug could make Motrin and Aleve obsolete."
The debate about hormone replacement therapy in women has been widely covered. The article by Francine Grodstein et al., "Hormone therapy and coronary heart disease: The role of time since menopause and age at hormone initiation,"
Journal of Women's Health
15 (2006), pp. 3544, sparked considerable news coverage. For insight into how the lay press reports laboratory and clinical studies, see Edward W Campion, "Medical research and the news media,"
NEJM
351 (2004), pp. 24362437. In the chapter, the
New York Times
article "Rethinking hormones, again," by Roni Rabin, appeared on January 31, 2006, and the
Wall Street Journal
article "In study of women's health, design flaws raise questions," by Tara Parker-Pope, on February 28, 2006.
Numerous articles in newspapers and magazines have alerted patients to marketing practices and the influence of consulting fees and gifts on physicians' advice: Abigail Zuger, "How tightly do ties between doctor and drug company bind?,"
New York Times,
July 27, 2006; Gina Kolata, "Spinal cement draws patients and questions,"
New York Times,
August 28, 2005; Gina Kolata, "With costs rising, treating back pain often seems futile,"
New York Times,
February 9, 2004; Reed Abelson, "Whistle-blower suit says device maker generously rewards doctors,"
New York Times,
January 24, 2006; Gardiner Harris, "In article, doctors back ban on gifts from drug makers,"
New York Times,
January 25, 2006; Carl Elliott, "The drug pushers,"
Atlantic Monthly,
April 2006; Gwen I fill interview with Dr. David Blumenthal, "Debating drug company gifts,"
PBS Online,
January 25, 2006.
The debate about the proper diagnosis and treatment of back pain can be found in the excellent review by Richard A. Deyo and James N. Weinstein, "Low back pain,"
NEJM
344 (2001), pp. 363–370. Also see Peter Fritzell et al., "Lumbar fusion versus nonsurgical treatment for chronic low back pain,"
Spine
26 (2001), pp. 2521–2534; Judith A. Turner et al., "Patient outcomes after lumbar spinal fusions,"
JAMA
268 (1992), pp. 907–911; Daniel C. Cherkin et al., "Physician variation in diagnostic testing for low back pain: Who you see is what you get,"
American College of Rheumatology
37 (1994), pp. 15–22. In the lay press, see Judy Foreman, "Aching spine,"
Boston Globe,
May 3, 2005. An important study about informed decision-making can be found in Richard A. Deyo et al., "Involving patients in clinical decisions: Impact of an interactive video program on use of back surgery,"
Medical Care
38 (2000), pp. 959–969.
10. In Service of the Soul
Stephen Hall's book is
A Commotion in the Blood: Life, Death, and the Immune System
(New York: Owl Books, 1998).
Readers interested in the history of medical philanthropy by the Rockefeller family should read Ron Chernow,
Titan: The Life of John D. Rockefeller, Sr.
(New York: Random House, 1998).
The IPSS was published in Peter Greenberg et al., "International scoring system for evaluating prognosis in myelodysplastic syndromes,"
Blood
89 (1997), pp. 2079–2088.
Epilogue
Dr. Arthur J. Barsky has written extensively about somatic symptoms caused by psychological distress. His work and that of others is featured in my article "Sick with worry: Can hypochondria be cured?,"
New Yorker,
August 11, 2003. Barsky and Emily C. Deans recently published a book for people suffering from hypochondria which sets out a program in cognitive behavioral therapy to ameliorate their suffering:
Stop Being Your Symptoms and Start Being Yourself
(New York: HarperCollins, 2006).
The study of forty-five doctors is by Derjung M. Tarn et al., "Physician communication when prescribing new medications,"
Archives of Internal Medicine
166 (2006), pp. 1855–1862.
The vignette told by Karen Delgado about the purple pills shows that system-wide solutions still require communication and are not default remedies for errors in care. Doctors have to keep thinking until they find the answer.
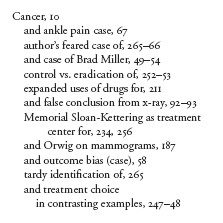
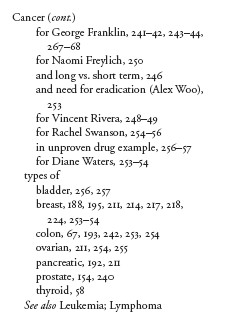
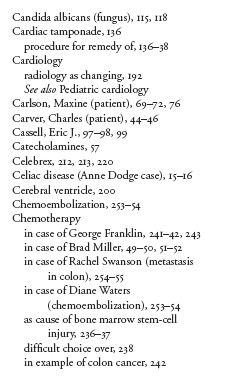
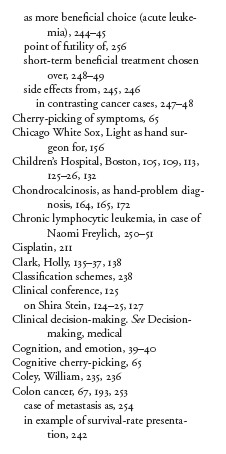
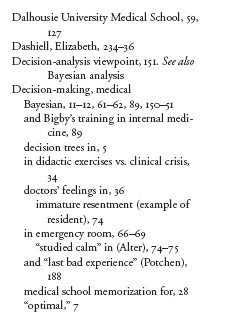
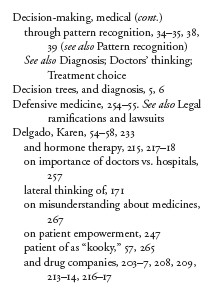
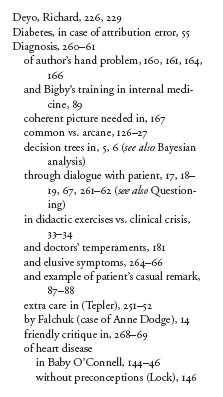
Index