Examination Medicine: A Guide to Physician Training (26 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

The classification of pulmonary hypertension was revised in 2008. The Venice classification is now called the Dana Point classification. The term ‘primary pulmonary hypertension’ has been replaced with ‘idiopathic pulmonary hypertension’ (see
Table 6.14
).
Table 6.14
The Dana Point classification for pulmonary hypertension (2008)
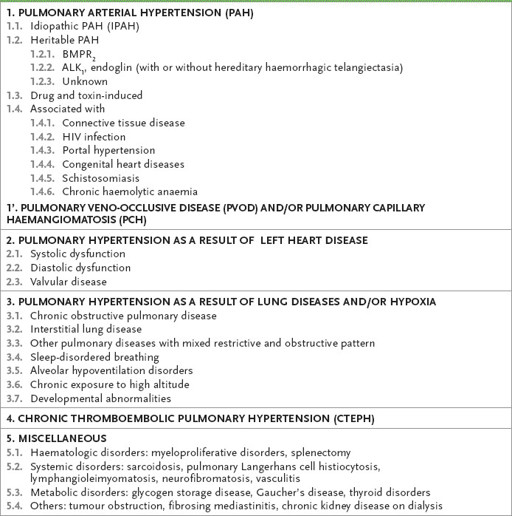
ALK
1
= activin receptor-like kinase type 1
BMPR = bone morphogenetic protein receptor type 2
HIV = human immunodeficiency virus
Adapted from G Simonneau, IM Robbins, M Beghetti, RN Channick et al. Updated clinical classification of pulmonary hypertension.
J Am Coll Cardiol
2009;54: S43–54.
The history
1.
Symptoms are usually non-specific but often severe. As usual, begin by asking whether the patient knows what is wrong and the reason for the admission, or visit, to hospital.
2.
If pulmonary hypertension seems a possibility, ask about the possible causes (
Table 6.14
). Remember to ask specifically about appetite-suppressing drugs. The use of fenfluramine and phenermine in combination and for long periods has been associated with the greatest risk.
3.
If the patient has an illness that could be a cause, ask detailed questions about that condition, its severity and chronicity. There may be a family history in cases of IPH (6%; autosomal dominant condition with incomplete penetrance, 20–80%). The majority of familial cases are associated with a mutation on the
BMPR2
gene.
4.
Find out how symptomatic the patient is now. Idiopathic and secondary pulmonary hypertension cause dyspnoea. Almost all patients have dyspnoea at the time of diagnosis. Other less common symptoms include fatigue, chest pain, syncope and oedema. Cough and haemoptysis can be present. Ask about symptoms of connective tissue diseases and especially about scleroderma. Try to work out the patient’s functional class (NYHA I–IV, often called the NYHA-WHO class when related to pulmonary hypertension).
5.
Ask about previous or planned investigations. These may relate to the underlying condition; for example, respiratory function tests or scans, echocardiography (often transoesophageal echocardiography) or cardiac catheterisation. A patient who presents with symptoms and signs of pulmonary hypertension needs a number of investigations before IPH can be diagnosed.
6.
What general treatment has been recommended? This may be for the underlying cardiac or respiratory condition or for thrombosis. There may be a history of cardiac surgery in childhood for congenital heart disease. Oxygen supplementation is often prescribed. Find out how this is administered (e.g. via nasal prongs or a mask), for how many hours a day and whether it comes from a concentrator or oxygen tanks. Oxygen is very expensive unless subsidised. Ask about the cost and inconvenience of the treatment with regard to portability and noise (oxygen concentrators are noisy and use a lot of electricity). Has the treatment been helpful?
7.
What drugs is the patient taking? Heparin and then warfarin are routine for pulmonary embolism, but warfarin is also used for many patients with IPH because of the risk of in situ thrombosis in the pulmonary arteries. Bronchodilators and steroids may have been prescribed for lung disease. The possibility of a heart or lung transplant, or both, may have been raised with the patient. The patient may be on a therapeutic trial or taking an agent, such as bosentan, sildenafil or the inhaled prostacyclin analogue iloprost. Patients involved in trials or taking new drugs are often very well informed about what is going on.
8.
As with any chronic and possibly debilitating condition, questions about the patient’s ability to work and manage the activities of daily living need to be detailed and comprehensive.
The examination
1.
Try to assess the severity of the patient’s dyspnoea as he or she undresses or by asking the patient to walk around the room.
2.
Perform a thorough respiratory and cardiac examination (see
Table 16.1, p. 311
and
Table 16.10, p. 342
). Look particularly for an elevated JVP with a large v wave. Feel for a parasternal impulse (right ventricular heave). Feel for a palpable P2 (and listen for tricuspid regurgitation).
3.
Look for signs of chronic lung disease, congenital heart disease and connective tissue disease. Examine for signs of a deep venous thrombosis (DVT).
Investigations
Investigations are directed at finding an underlying reason for pulmonary hypertension – IPH is a diagnosis of exclusion – and at assessing its severity and potential reversibility. These investigations include those detailed below.
1.
Chest X-ray
– this will be abnormal in 90% of IPH patients. It may show ILD or an abnormal cardiac silhouette – right ventricular dilatation. There may be large proximal pulmonary arteries that appear ‘pruned’ in the periphery, and the right ventricle may appear enlarged on the lateral film (see
Fig 6.7a and b
).
FIGURE 6.7
(a) and (b) Severe pulmonary hypertension. There is pruning of the pulmonary arteries and right ventricular dilatation.
2.
Respiratory function tests
(normal, restrictive or obstructive pattern) – moderate pulmonary hypertension itself is associated with a reduction in the diffusion capacity for carbon monoxide (DLCO) to about 50% of predicted.
3.
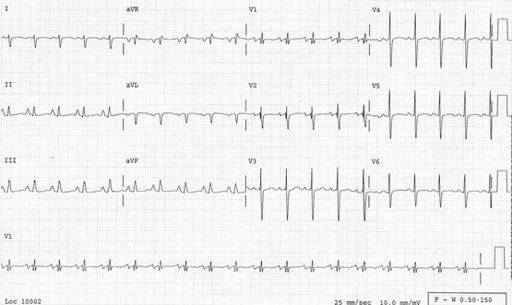
ECG
–
signs of right heart strain or hypertrophy are present in up to 90% of patients (see
Fig 6.8
).
FIGURE 6.8
ECG of a patient with idiopathic pulmonary hypertension. Note RAA (right atrial abnormality), ‘P’ pulmonale, right axis, right ventricular hypertrophy and strain pattern, and sinus tachycardia.
4.
Blood gases
– hypercapnia in hypoventilation syndromes, but hypocapnia is more common in IPH because of increased alveolar ventilation. Mild hypoxia in IPH, but more severe when pulmonary hypertension is secondary to lung disease.
5.
CT pulmonary angiogram or ventilation–perfusion (V/Q) scan and Doppler venograms
– DVT and pulmonary embolism – assessment of extent of involvement of the pulmonary bed.
6.
High-resolution CT of the lungs
– looking for interstitial lung disease.
7.
Six-minute walking test
– predicts survival and correlates with NYHA-WHO class. Reduction in arterial oxygen concentration of >10% during this test predicts almost threefold mortality risk over 29 months. Patients unable to manage 332 metres in 6 minutes also have an adverse prognosis.
8.
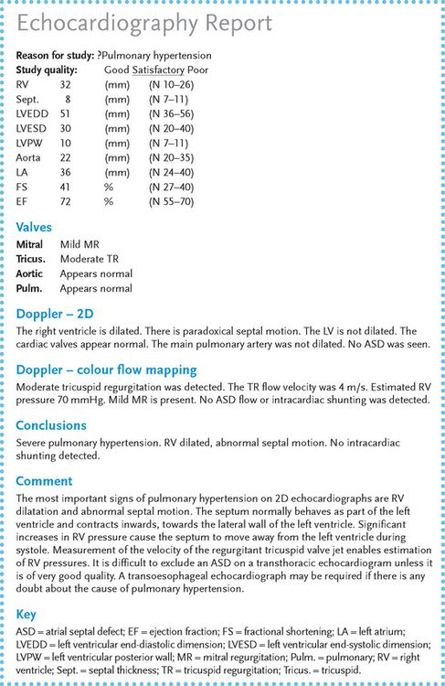
Transthoracic or transoesophageal echocardiogram
(see
Fig 6.9
) – a trans-thoracic echocardiogram will usually enable left ventricular failure or severe mitral valve disease to be excluded. One or both will enable the assessment of known congenital heart disease, the detection of a left to right (or reversed) shunting (Eisenmenger’s syndrome) and measurement, in many cases, of pulmonary artery pressures. The presence of tricuspid regurgitation (common in normal people and almost universal in the presence of raised right ventricular pressures) enables estimation of right ventricular, and therefore pulmonary artery, pressures in many patients. The pressure difference across the tricuspid valve can be calculated if the velocity of the regurgitant jet is measured by Doppler. Right atrial pressures are
usually close to 5 mmHg; the right ventricular pressure can be estimated by adding 5 to the pressure difference across the tricuspid valve. The normal right ventricular and pulmonary artery systolic pressure is 20–25 mmHg. Assessment of pulmonary artery ejection characteristics can also be used to estimate pulmonary artery pressures. Right ventricular size and function can be assessed. Right ventricular dilatation and abnormal septal motion are useful signs of pulmonary hypertension. The right ventricle appears abnormal on echocardiograms in more than 90% of people with pulmonary hypertension.
FIGURE 6.9
Echocardiography report in a patient with pulmonary hypertension.
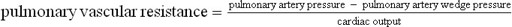
9.
Catheterisation of the right heart
– this investigation is the gold standard and should also be performed if other tests have not been definitive. It is usually performed with a multiple-lumen flotation catheter and enables direct measurement of the right heart pressures. Left to right shunting can be detected by the collection of blood samples from the venae cavae, right atrium, right ventricle and pulmonary artery. A ‘step-up’ in the blood oxygen saturation indicates a shunt. The size of the shunt can be calculated if the cardiac output is measured by thermo dilution. Measurement of the pulmonary artery wedge pressure enables the detection of mitral stenosis or the very rare pulmonary veno-occlusive disease. By definition, IPH means the pulmonary capillary wedge pressure is <18 mmHg (i.e. the raised pulmonary pressures are not secondary to left ventricular failure). Pulmonary vascular resistance can be calculated using the cardiac output, pulmonary artery pressure and pulmonary artery wedge pressure measurements. The formula is: