The Coming Plague (102 page)
Authors: Laurie Garrett

The same principles held true for
Anopheles
mosquitoes and the spread of malaria. In 1993, Uwe Brinkmann, who headed the Harvard Working Group on New and Resurgent Diseases, was trying to figure out ways to
predict not only latitude movements of mosquitoes in response to global warming but also their altitude changes. He felt there was an urgent need for research to determine which factors played a greater role in limiting
Anopheles
activities at altitudes above 500 feet: air pressure or cooler temperatures. If the latter was more important, he predicted, malaria could quickly overtake mountainous areas of Zimbabwe, Botswana, Swaziland, Rwanda, Tanzania, Kenya, and other geographically diverse parts of Africa. Further, the disease might with global warming climb its way further up the foothills of the Himalayas, the Sulaiman Range, the Pir Panjal, and other mountainous regions of Asia.
Anopheles
mosquitoes and the spread of malaria. In 1993, Uwe Brinkmann, who headed the Harvard Working Group on New and Resurgent Diseases, was trying to figure out ways to
predict not only latitude movements of mosquitoes in response to global warming but also their altitude changes. He felt there was an urgent need for research to determine which factors played a greater role in limiting
Anopheles
activities at altitudes above 500 feet: air pressure or cooler temperatures. If the latter was more important, he predicted, malaria could quickly overtake mountainous areas of Zimbabwe, Botswana, Swaziland, Rwanda, Tanzania, Kenya, and other geographically diverse parts of Africa. Further, the disease might with global warming climb its way further up the foothills of the Himalayas, the Sulaiman Range, the Pir Panjal, and other mountainous regions of Asia.
A detailed WHO Task Group report in 1990 offered a broader range of expected disease impacts from global warming. Even a moderate net temperature increaseâon the order of 1°Câwould alter wind patterns, change levels of relative humidity and rainfall, produce a rise in sea levels, and widen the global extremes between desert regions and areas afflicted with periodic flooding. These conditions would, in turn, radically alter the ecologies of microbes that were carried by insects. Furthermore, expected changes in vegetation patterns could, the WHO Task Group said, radically alter the ecologies of microbe-carrying animals, such as monkeys, rats, mice, and bats, bringing those vectors into closer proximity to
Homo sapiens
.
49
Homo sapiens
.
49
There was also a strong consensus among immunologists that heightened exposure to ultraviolet lightâparticularly UV-B radiationâsuppressed the human immune response, thus increasing
Homo sapiens
' susceptibility to all microbes.
50
Just as PCBs and other hydrocarbon pollutants were thought to have played a role in increasing microbial susceptibility in marine mammals, so many physicians felt there was ample evidence that air, water, and food pollutants affected the human immune system.
Homo sapiens
' susceptibility to all microbes.
50
Just as PCBs and other hydrocarbon pollutants were thought to have played a role in increasing microbial susceptibility in marine mammals, so many physicians felt there was ample evidence that air, water, and food pollutants affected the human immune system.
Another feature of global warming would be an increased dependence in wealthier nations on air conditioning. In order to conserve energy, buildings in the industrialized world had specifically been designed to minimize outward and inward air flow. It was much cheaper to heat or cool the same air repeatedly in a sealed room than to pump in fresh air from the outside, alter its temperature, circulate it throughout a structure, and at the same time expel old air. As the numbers of hot days per year increased, necessitating longer periods of reliance upon air conditioning, the economic pressures to recirculate old air repeatedly, to the limits of reasonable oxygen depletion, could be expected. Such practices for winter heat conservation in large office buildings had already been linked to workplace transmission of influenza and common cold viruses. Spread of Legionnaires' Disease and other airborne microbes was expected to increase with global warming.
Even in the absence of serious global warming, energy conservation practices were, for purely economic reasons, spurring architects and developers toward construction of buildings that lacked any openable windows and were sealed so tightly that residents were apt to suffer “sick building
syndrome”: the result of inhaling formaldehyde, radon, and other chemicals present in the building foundation or structure. Such chemicals posed little threat to human health if diluted in fresh air, but were significant contributors to health problems in residents and employees who inhaled levels that were concentrated in recirculated or thin air. Obviously, a building that was capable of concentrating such trace chemicals in the air breathed by its inhabitants would also serve as an ideal setting for rapid dissemination of
Mycobacterium tuberculosis,
if an individual who suffered from active pulmonary disease was residing or working within the structure.
syndrome”: the result of inhaling formaldehyde, radon, and other chemicals present in the building foundation or structure. Such chemicals posed little threat to human health if diluted in fresh air, but were significant contributors to health problems in residents and employees who inhaled levels that were concentrated in recirculated or thin air. Obviously, a building that was capable of concentrating such trace chemicals in the air breathed by its inhabitants would also serve as an ideal setting for rapid dissemination of
Mycobacterium tuberculosis,
if an individual who suffered from active pulmonary disease was residing or working within the structure.
The human lung, as an ecosphere, was designed to take in 20,000 liters of air each day, or roughly 60 pounds. Its surface was highly variegated, comprised of hundreds of millions of tiny branches, at the ends of which were the minute bronchioles that actively absorbed oxygen molecules. The actual surface area of the human lung was, therefore, about 150 square meters, or “about the size of an Olympic tennis court,” as Harvard Medical School pulmonary expert Joseph Brain put it.
Less than 0.64 micron, or just under one one-hundred-thousandth of an inch, was all the distance that separated the air environment in the lungs from the human bloodstream.
All a microbe had to do to gain entry to the human bloodstream was get past that 0.64 micron of protection. Viruses accomplished the task by accumulating inside epithelial cells in the airways and creating enough local damage to open up a hole of less than a millionth of an inch in diameter. Some viruses, such as those that caused common colds, were so well adapted to the human lung that they had special proteins on their surfaces which locked on to the epithelial cells. Larger microbes, such as the tuberculosis bacteria, gained entry via the immune system's macrophages. They were specially adapted to recognize and lock on to the large macrophages that were distributed throughout pulmonary tissue. Though it was the job of macrophages to seek out and destroy such invaders, many microbes had adapted ways to fool the cells into ingesting them. Once inside the macrophages, the microbes got a free ride into the blood or the lymphatic system, enabling them to reach destinations all over the human body.
The best way to protect the lungs was to provide them with 20,000 liters per day of fresh, clean, oxygen-rich air. The air flushed out the system.
Dirty airâthat which contained pollutant particles, dust, or microbes âassaulted the delicate alveoli and bronchioles, and there was a synergism of action. People who, for example, smoked cigarettes or worked in coal mines were more susceptible to all respiratory infectious diseases: colds, flu, tuberculosis, pneumonia, and bronchitis.
Because of its confined internal atmosphere, the vehicle responsible for the great globalization of humanityâthe jet airplaneâcould be a source of microbial transmission. Everybody on board an airplane shared the same air. It was, therefore, easy for one ailing passenger or crew member to pass
a respiratory microbe on to many, if not all, on board. The longer the flight, and the fewer the number of air exchanges in which outside air was flushed through the cabin, the greater the risk.
a respiratory microbe on to many, if not all, on board. The longer the flight, and the fewer the number of air exchanges in which outside air was flushed through the cabin, the greater the risk.
In 1977, for example, fifty-four passengers were grounded together for three hours while their plane underwent repairs in Alaska. None of the passengers left the aircraft, and to save fuel the air conditioning was switched off. For three hours the fifty-four passengers breathed the same air over and over again. One woman had influenza: over the following week 72 percent of her fellow passengers came down with the flu; genetically identical strains were found in everyone.
51
51
Following the worldwide oil crisis of the 1970s, the airlines industry looked for ways to reduce fuel use. An obvious place to start was with air circulation, since it cost a great deal of fuel to draw icy air in from outside the aircraft, adjust its temperature to a comfortable 65°â70°F, and maintain cabin pressure. Prior to 1985 commercial aircraft performed that function every three minutes, which meant most passengers and crew breathed fresh air throughout their flight. But virtually all aircraft built after 1985 were specifically designed to circulate air less frequently; a mix of old and fresh air circulated once every seven minutes, and total flushing of the aircraft could take up to thirty minutes.
52
Flight crews increasingly complained of dizziness, flu, colds, headaches, and nausea.
52
Flight crews increasingly complained of dizziness, flu, colds, headaches, and nausea.
Studies of aircraft cabins revealed excessive levels of carbon dioxideâup to 50 percent above U.S. legal standards. Air quality for fully booked airliners failed to meet any basic standards for U.S. workplaces.
53
53
In 1992 and 1993 the CDC investigated four instances of apparent transmission of tuberculosis aboard aircraft. In one case, a flight attendant passed TB on to twenty-three crew members over the course of several flights.
Similar concerns regarding confined spaces were raised about institutional settings, such as prisons and dormitories, where often excessive numbers of people were co-housed in energy-efficient settings.
In preparation for the June 1992 United Nations Earth Summit in Rio de Janeiro, the World Health Organization reviewed available data on expected health effects of global warming and pollution.
54
WHO concluded that evidence of increased human susceptibility to infectious diseases, due to UV-B immune system damage and pollutant impacts on the lungs and immune system, was compelling. The agency was similarly impressed with estimates of current and projected changes in the ecology of disease vectors, particularly insects.
54
WHO concluded that evidence of increased human susceptibility to infectious diseases, due to UV-B immune system damage and pollutant impacts on the lungs and immune system, was compelling. The agency was similarly impressed with estimates of current and projected changes in the ecology of disease vectors, particularly insects.
It wasn't necessary, of course, for the earth to undergo a 1°â5°C temperature shift in order for diseases to emerge. As events since 1960 had demonstrated, other, quite contemporary factors were at play. The ecological relationship between
Homo sapiens
and microbes had been out of balance for a long time.
Homo sapiens
and microbes had been out of balance for a long time.
The “disease cowboys”âscientists like Karl Johnson, Pierre Sureau,
Joe McCormick, Peter Piot, and Pat Webbâhad long ago witnessed the results of human incursion into new niches or alteration of old niches.
55
Perhaps entomologist E. O. Wilson, when asked, “How many disease-carrying reservoir and vector species await discovery in the earth's rain forests?” best summed up the predicament: “That is unknown and unknowable. The scale of the unknown is simply too vast to even permit speculation.”
Joe McCormick, Peter Piot, and Pat Webbâhad long ago witnessed the results of human incursion into new niches or alteration of old niches.
55
Perhaps entomologist E. O. Wilson, when asked, “How many disease-carrying reservoir and vector species await discovery in the earth's rain forests?” best summed up the predicament: “That is unknown and unknowable. The scale of the unknown is simply too vast to even permit speculation.”
Â
Thanks to changes in
Homo sapiens
activities, in the ways in which the human species lived and worked on the planet at the end of the twentieth century, microbes no longer remained confined to remote ecospheres or rare reservoir species: for them, the earth had truly become a Global Village. Between 1950 and 1990 the number of passengers aboard international commercial air flights soared from 2 million to 280 million. Domestic passengers flying within the United States reached 424 million in 1990.
56
Infected human beings were moving rapidly about the planet, and the number of air passengers was expected to double by the year 2000, approaching 600 million on international flights.
57
Homo sapiens
activities, in the ways in which the human species lived and worked on the planet at the end of the twentieth century, microbes no longer remained confined to remote ecospheres or rare reservoir species: for them, the earth had truly become a Global Village. Between 1950 and 1990 the number of passengers aboard international commercial air flights soared from 2 million to 280 million. Domestic passengers flying within the United States reached 424 million in 1990.
56
Infected human beings were moving rapidly about the planet, and the number of air passengers was expected to double by the year 2000, approaching 600 million on international flights.
57
Once microbes reached new locales, increasing human population and urbanization ensured that even relatively poorly transmissible microbes faced ever-improving statistical odds of being spread from person to person. The overall density of average numbers of human beings residing on a square mile of land on the earth rose steadily every year. In the United States, even adjusting for the increased land mass of the country over time, density (according to U.S. census figures) rose as follows:
| Year | Total Population | Persons per Square Mile |
|---|---|---|
| 1790 | 3,929,214 | 4.5 |
| 1820 | 9,638,453 | 5.5 |
| 1850 | 23,191,876 | 7.9 |
| 1870 | 39,818,449 | 13.4 |
| 1890 | 62,947,714 | 21.2 |
| 1910 | 91,972,266 | 31.0 |
| 1930 | 122,775,046 | 41.2 |
| 1950 | 151,325,798 | 42.6 |
| 1970 | 203,211,926 | 57.5 |
| 1990 | 250,410,000 | 70.3 |
| 1992 | 256,561,239 | 70.4 |
Â
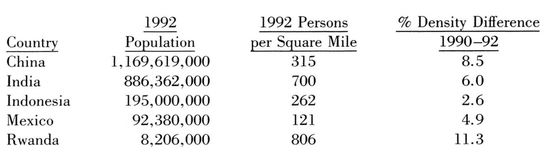
In most of the world the observed increases were even more dramatic. In a comparison of 1990 and 1992 census information as collected by the United Nations, the two-year upward trend in population density was unmistakable:
| Country | 1990 Population | 1990 Persons per Square Mile |
|---|---|---|
| China | 1,130,065,000 | 288 |
| India | 850,067,000 | 658 |
| Indonesia | 191,266,000 | 255 |
| Mexico | 88,335,000 | 115 |
| Rwanda | 7,603,000 | 715 |
Other books
The Tunnel by Eric Williams
Liberator by Bryan Davis
Catt Chasing by Shana Burton
In Paradise by Blaise, Brit
Ray Bradbury Stories, Volume 1 by Ray Bradbury
Yours or Mine by Craver, D.S.
Cover Model by Devon Hartford
Sweetest Sorrow (Forbidden Book 2) by J.M. Darhower
